Hidradenitis suppurativa
| Hidradenitis suppurativa | |
|---|---|
| Other names | Acne inversa, apocrine acne, Verneuil's disease, Velpeau's disease[1] |
 | |
| Hidradenitis suppurativa (Hurley's stage II) in the left armpit. | |
| Specialty | Dermatology |
| Symptoms | Multiple inflamed and swollen skin lesions[2] |
| Usual onset | Childhood and Young adulthood[2] |
| Duration | Long-term[2] |
| Types | Stage I, II, III[1] |
| Causes | Unknown[3] |
| Diagnostic method | Based on symptoms[2] |
| Differential diagnosis | Acne, acne conglobata, pilonidal cysts[2] |
| Treatment | Warm baths, laser therapy, surgery[2][4] |
| Medication | Secukinumab, antibiotics, immunosuppressive medication[2] |
| Frequency | 1–4% of people, when mild cases are included[2][3] |
| Deaths | Rare[1] |


Hidradenitis suppurativa (HS), sometimes known as acne inversa or Verneuil's disease, is a long-term dermatological condition characterized by the occurrence of inflamed and swollen lumps.[2][3] These are typically painful and break open, releasing fluid or pus.[3] The areas most commonly affected are the underarms, under the breasts, perineum, buttocks, and the groin.[1] Scar tissue remains after healing.[1] HS may significantly limit many everyday activities, for instance, walking, hugging, moving, and sitting down. Sitting disability may occur in patients with lesions in sacral, gluteal, perineal, femoral, groin or genital regions; and prolonged periods of sitting down can also worsen the condition of the skin of these patients.[5][6][7][8][9]
The exact cause is usually unclear, but believed to involve a combination of genetic and environmental factors.[3] About a third of people with the disease have an affected family member.[3] Other risk factors include obesity and smoking.[3] The condition is not caused by an infection, poor hygiene, or the use of deodorant.[3][4] Instead, it is believed to be caused by hair follicles being obstructed,[10][1] with the nearby apocrine sweat glands being strongly implicated in this obstruction.[1][11] The sweat glands themselves may or may not be inflamed.[1] Diagnosis is based on the symptoms.[2]
No cure is known,[4] though surgical excision with wet-to-dry dressings, proper wound care, and warm baths or showering with a pulse-jet shower may be used in those with mild disease.[4] Cutting open the lesions to allow them to drain does not result in significant benefit.[2] While antibiotics are commonly used, evidence for their use is poor.[4] Immunosuppressive medication may also be tried.[2] In those with more severe disease, laser therapy or surgery to remove the affected skin may be viable.[2] Rarely, a skin lesion may develop into skin cancer.[3]
If mild cases of HS are included, then the estimate of its frequency is from 1–4% of the population.[2][3] Women are three times more likely to be diagnosed with it than men.[2] Onset is typically in young adulthood and may become less common after 50 years old.[2] It was first described between 1833 and 1839 by French anatomist Alfred Velpeau.[1][12]
Terminology
[edit]Although hidradenitis suppurativa is often referred to as acne inversa, it is not a form of acne, and lacks the core defining features of acne such as the presence of closed comedones and increased sebum production.[13]
Causes
[edit]The exact cause of hidradenitis suppurativa remains unknown,[11][14] and there has, in the recent past, been notable disagreement among experts in this regard.[15] The condition, however, likely stems from both genetic and environmental causes.[3] Specifically, an immune-mediated pathology has been proposed,[11] although environmental factors have not been ruled out.[3]
Lesions will occur in any body areas with hair follicles,[15] and/or sweat glands,[16] although areas such as the axilla, groin, and perineal region are more commonly involved. This theory includes most of these potential indicators:[17]
- Post-pubescent individuals[18]
- Blocked hair follicles or blocked apocrine sweat glands
- Excessive sweating
- Androgen dysfunction
- Genetic disorders that alter cell structure
The historical understanding of the disease suggests dysfunctional apocrine glands[19] or dysfunctional hair follicles,[20] possibly triggered by a blocked gland, which creates inflammation, pain, and a swollen lesion.
Triggering factors
[edit]Several triggering factors should be taken into consideration:
- Obesity[21] is an exacerbating rather than a triggering factor,[22] through mechanical irritation, occlusion, and skin maceration.
- Tight clothing,[21] and clothing made of heavy, nonbreathable materials[23]
- Deodorants, depilation products, shaving of the affected area – their association with HS is still an ongoing debate among researchers.[24]
- Drugs, in particular oral contraceptive pills,[25] cigarette smoking,[26][27] and lithium.[28]
- Hot and especially humid climates.[29]
- Stress[27]
Predisposing factors
[edit]- Genetic factors:[22] an autosomal dominant inheritance pattern has been proposed.[30]
- Endocrine factors:
- Sex hormones, especially an excess of androgens, are thought to be involved, although the apocrine glands are not sensitive to these hormones.[31] Women often have outbreaks before their menstrual period and after pregnancy; HS severity usually decreases during pregnancy and after menopause.
- Diabetes mellitus is common in hidradenitis suppurativa and seems to be a risk factor.[32]
Some cases have been found to result from mutations in the NCSTN, PSEN1, or PSENEN genes. The genes produce proteins that are all components of a complex called gamma- (γ-) secretase. This complex cuts apart (cleaves) many different proteins, which is an important step in several chemical signaling pathways. One of these pathways, known as notch signaling, is essential for the normal maturation and division of hair follicle cells and other types of skin cells. Notch signaling is also involved in normal immune system function. Studies suggest that mutations in the NCSTN, PSEN1, or PSENEN gene impair notch signaling in hair follicles. Although little is known about the mechanism, abnormal notch signaling appears to promote the development of nodules and to lead to inflammation in the skin.[33] In addition, the composition of the intestinal microflora and as a consequence dietary patterns appear to play a role. Although dysbiosis of the cutaneous microbiome apparent in HS is not observed, the concurrent existence of inflammatory gut and skin diseases has led to the postulation of a gut-skin axis in which gut microbiota is implicated. Indeed, analysis of bacterial taxa in fecal samples from HS patients support the possibility of a role for intestinal microbial alterations in this chronic inflammatory skin disease.[34]
Precocious puberty is more common among children and adolescents with hidradenitis suppurativa (HS) compared to those without the condition, according to a recent case-control study.[35] An analysis of the Explorys database revealed that pediatric patients with precocious puberty have double the risk of developing HS, even after adjusting for factors like demographic characteristics and body mass index (BMI).[36]
Diagnosis
[edit]Early diagnosis is essential in avoiding tissue damage. However HS is often misdiagnosed or diagnosed late due to healthcare professionals not being aware of the condition or people not consulting with a physician.[37][38] Globally, the diagnosis is delayed more than 7 years in average after symptoms appear. This is much longer than with other skin conditions.[39]
Stages
[edit]

Hidradenitis suppurativa presents itself in three stages.[19][41] Due to the large spectrum of clinical severity and the severe impact on quality of life, a reliable method for evaluating HS severity is needed.[citation needed]
Hurley's staging system
[edit]Hurley's staging system was the first classification system proposed, and is still in use for the classification of patients with skin diseases (i.e., psoriasis, HS, acne). Hurley separated patients into three groups based largely on the presence and extent of cicatrization and sinuses. It has been used as a basis for clinical trials in the past and is a useful basis to approach therapy for patients. These three stages are based on Hurley's staging system, which is simple and relies on the subjective extent of the diseased tissue the patient has. Hurley's three stages of hidradenitis suppurativa are:[42]
| Stage | Characteristics |
|---|---|
| I | Solitary or multiple isolated abscess formation without scarring or sinus tracts (A few minor sites with rare inflammation; may be mistaken for acne.) |
| II | Recurrent abscesses, single or multiple widely separated lesions, with sinus tract formation (Frequent inflammation restricts movement and may require minor surgery such as incision and drainage.) |
| III | Diffuse or broad involvement across a regional area with multiple interconnected sinus tracts and abscesses (Inflammation of sites to the size of golf balls, or sometimes baseballs; scarring develops, including subcutaneous tracts of infection – see fistula. Obviously, patients at this stage may be unable to function.) |
Sartorius staging system
[edit]The Sartorius staging system is more sophisticated than Hurley's. Sartorius et al. suggested that the Hurley system is not sophisticated enough to assess treatment effects in clinical trials during research. This classification allows for better dynamic monitoring of the disease severity in individual patients. The elements of this staging system are:[43]
- Anatomic regions involved (axilla, groin gluteal, or other region or inframammary region left or right)
- Number and types of lesions involved (abscesses, nodules, fistulas or sinuses, scars, points for lesions of all regions involved)
- The distance between lesions, in particular the longest distance between two relevant lesions (i.e., nodules and fistulas in each region or size if only one lesion present)
- The presence of normal skin in between lesions (i.e., if all lesions are clearly separated by normal skin)
Points are accumulated in each of the above categories, and added to give both a regional and total score. In addition, the authors recommend adding a visual analog scale for pain or using the dermatology life quality index (DLQI, or the 'skindex') when assessing HS.[44]
Treatment
[edit]Treatment depends upon presentation and severity of the disease. Due to the poorly studied nature of the disease, the effectiveness of drugs and therapies were unclear.[45] Clear and sensitive communication from health care professionals, social and psychological interventions can help managing the emotional impact of the condition and aid necessary lifestyle changes.[37][38] In May 2023, the European Commission (EC) approved Cosentyx (secukinumab) for active moderate to severe hidradenitis suppurativa in adults.[46]
Other possible treatments include the following:
Cryotherapy
[edit]Cryotherapy has demonstrated efficacy against the disease, with 88% of persistent lesions resolving in a clinical trial of 23 patients.[47]
Lifestyle
[edit]Warm baths may be tried in those with mild disease.[4] Weight loss and the cessation of smoking are also recommended.[2]
Medication
[edit]- Antibiotics: taken by mouth, these are used for their anti-inflammatory properties rather than to treat infection. Most effective is a combination of rifampicin and clindamycin given concurrently for 2–3 months. Popular antibiotics also include tetracycline and minocycline.[48] Topical clindamycin has been shown to have an effect in double-blind placebo controlled studies.[49] In a retrospective review and telephone survey, intravenous ertapenem therapy showed clinical improvement with 80.3% of subjects reporting medium to high satisfaction and 90.8% would recommend ertapenem to other patients.[50]
- Corticosteroid injections, also known as intralesional steroids, can be particularly useful for localized disease, if the drug can be prevented from escaping via the sinuses.
- Antiandrogen therapy, hormonal therapy with antiandrogenic medications such as spironolactone, flutamide, cyproterone acetate, ethinylestradiol, finasteride, dutasteride, and metformin, have been found to be effective in clinical studies.[51][52][53] However, the quality of available evidence is low and does not presently allow for robust evidence-based recommendations.[51][52]
- Intravenous infusion or subcutaneous injection of anti-inflammatory (TNF inhibitors; anti-TNF-alpha) drugs such as infliximab, and etanercept[54] This use of these drugs is not currently Food and Drug Administration (FDA) approved and is somewhat controversial, so may not be covered by insurance.
- Biologics: Studies have supported that various biologics have a positive effect on HS lesions.[55] Specifically adalimumab at weekly intervals is useful.[56] Adalimumab and Secukinumab[57][58] are both approved by the FDA for the treatment of HS as of 2023.
- Topical isotretinoin is usually ineffective in people with HS, and is more commonly known as a medication for the treatment of acne vulgaris. Individuals affected by HS who responded to isotretinoin treatment tended to have milder cases of the condition.[59]
- Zinc and Nicotinamide, at doses of 90 mg and 30 mg respectively, have shown efficacy against mild to moderate hidradenitis suppurativa in a controlled retrospective clinical trial.[60]
Surgery
[edit]When the process becomes chronic, wide surgical excision is the procedure of choice.
Wounds in the affected area do not heal by secondary intention, and immediate or delayed application of a split-thickness skin graft is an option.[17] Another option is covering the defect with a perforator flap. With this technique, the (mostly totally excised) defect is covered with tissue from an area nearby. For example, the axilla with a fully excised defect of 15 × 7 cm can be covered with a thoracodorsal artery perforator flap.[citation needed]. A less invasive excision procedure called Skin-Tissue-sparing Excision with Electrosurgical Peeling or "STEEP" has also been developed for treating moderate to severe disease.[61]
Laser hair removal
[edit]The 1064-nm wavelength laser for hair removal may aid in the treatment of HS.[62] A randomized control study has shown improvement in HS lesions with the use of a Nd:YAG laser.[63]
Botox injection
[edit]A 2022 study reported that administration of Botulinum toxin resulted in either clinical improvement or improved quality of life in 96.8% (n = 30/31) of HS patients. Level of evidence was moderate. It concluded that the treatment was a safe and potentially effective alternative for hidradenitis suppurativa patients resistant to standard of care therapies.[64]
Prognosis
[edit]
In stage III disease, as classified by the Hurley's staging system, fistulae left undiscovered, undiagnosed, or untreated, can rarely lead to the development of squamous cell carcinoma in the anus or other affected areas.[65][66] Other stage III chronic sequelae may also include anemia, multilocalized infections, amyloidosis, and arthropathy. Stage III complications have been known to lead to sepsis, but clinical data are still uncertain.

Potential complications
[edit]- Contractures and reduced mobility of the lower limbs and axillae due to fibrosis and scarring occur. Severe lymphedema may develop in the lower limbs.
- Local and systemic infections (meningitis, bronchitis, pneumonia, etc.), are seen, which may even progress to sepsis.
- Higher risk for diabetes mellitus.[32] Treatment of HS may contribute to remission of diabetes.[67]
- Interstitial keratitis
- Anal, rectal, or urethral fistulae[68]
- Normochromic or hypochromic anemia[69]
- People with HS may be at increased risk for autoimmune disorders including ankylosing spondylitis, rheumatoid arthritis, and psoriatic arthritis.[70]
- Squamous cell carcinoma has been found on rare occasions in chronic hidradenitis suppurativa of the anogenital region.[71] The mean time to the onset of this type of lesion is 10 years or more and the tumors are usually highly aggressive.
- Tumors of the lung and oral cavity, and liver cancer[72]
- Hypoproteinemia and amyloidosis, which can lead to kidney failure and death[73]
- Seronegative and usually asymmetric arthropathy: pauciarticular arthritis, polyarthritis/polyarthralgia syndrome[74]
Impact on mental health
[edit]HS is a painful and socially isolating condition which leads to a negative impact on mental health as well. A 2020 meta-analysis found that 21% of people with HS have depression and 12% have anxiety.[75] A 2020 study found that people with HS have suicide rates more than double the rates in controls, and also have a higher risk of attempting suicide.[76]
Epidemiology
[edit]Prevalence
[edit]Estimates of the prevalence of HS vary worldwide and there is no accepted generalization. In the USA, the prevalence is estimated to be 0.1% while in Europe it is thought to be 1% or more.[76]
Gender
[edit]In North America and Europe, women are three times more likely to have HS. However, in South Korea, men are twice as likely to have HS.[76]
Age
[edit]HS is the most prevalent in people in their 40s and 50s.[76]
Comorbidities
[edit]Especially endocrine diseases are more common in HS.[77] Diabetes mellitus may be both a causal factor contributing to the evolution and/or severity of HS and a consequence of inflammation in HS.[32][67] Thyroid disorders are more common, too, in HS.[78]
History
[edit]- From 1833 to 1839, in a series of three publications, Velpeau identified and described a disease now known as hidradenitis suppurativa.[79]
- In 1854, Verneuil described hidradenitis suppurativa as hidrosadénite Phlegmoneuse. This is how HS obtained its alternate name "Verneuil's disease".[80]
- In 1922, Schiefferdecker hypothesized a pathogenic link between "acne inversa" and human sweat glands.[81]
- In 1956, Pillsbury et al.[82] coined the term follicular occlusion triad for the common association of hidradenitis suppurativa, acne conglobata and dissecting cellulitis of the scalp. Modern clinical research still employs Pillsbury's terminology for these conditions' descriptions.[83]
- In 1975, Plewig and Kligman, following Pillsbury's research path, modified the "acne triad", replacing it with the "acne tetrad: acne triad, plus pilonidal sinus".[84] Plewig and Kligman's research follows in Pillsbury's footsteps, offering explanations of the symptoms associated with hidradenitis suppurativa.
- In 1989, Plewig and Steger's research led them to rename hidradenitis suppurativa, calling it "acne inversa" – which is not still used today in medical terminology, although some individuals still use this outdated term.[85]
A surgeon from Paris, Velpeau described an unusual inflammatory process with formation of superficial axillary, submammary, and perianal abscesses, in a series of three publications from 1833 to 1839. One of his colleagues, also located in Paris, named Verneuil, coined the term hidrosadénite phlegmoneuse about 15 years later. This name for the disease reflects the former pathogenetic model of acne inversa, which is considered inflammation of sweat glands as the primary cause of hidradenitis suppurativa. In 1922, Schiefferdecker suspected a pathogenic association between acne inversa and apocrine sweat glands. In 1956, Pillsbury postulated follicular occlusion as the cause of acne inversa, which they grouped together with acne conglobata and perifolliculitis capitis abscendens et suffodiens ("dissecting cellulitis of the scalp") as the "acne triad". Plewig and Kligman added another element to their acne triad, pilonidal sinus. Plewig et al. noted that this new "acne tetrad" includes all the elements found in the original "acne triad", in addition to a fourth element, pilonidal sinus. In 1989, Plewig and Steger introduced the term "acne inversa", indicating a follicular source of the disease and replacing older terms such as "Verneuil disease".
| Author | Year | Findings |
|---|---|---|
| Velpeau | 1839 | First description of the hidradenitis suppurativa |
| Verneuil | 1854 | "Hidrosadénite phlegmoneuse" |
| Pillsbury | 1956 | Acne triad (hidradenitis suppurativa, perifolliculitis capitis abscendens et suffodiens, acne congoblata) |
| Plewig & Kligman | 1975 | Acne tetrad (acne triad + pilonidal sinus) |
| Plewig & Steger | 1989 | Acne inversa |
Other names
[edit]Hidradenitis suppurativa has been referred to by multiple names in the literature, as well as in various cultures. Some of these are also used to describe different diseases, or specific instances of this disease.[41]
- Acne conglobata – not really a synonym – this is a similar process, but in classic acne areas of chest and back
- Acne inversa – a proposed new term[86][87] which has not gained widespread favor.[88]
- Apocrine acne – an outdated term based on the disproven[citation needed] concept that apocrine glands are primarily involved, though many do have apocrine gland infection
- Apocrinitis – another outdated term based on the same thesis
- Fox-den disease – a term not used in medical literature, based on the deep fox den–like sinuses
- Hidradenitis supportiva – a misspelling
- Pyodermia fistulans significa – now considered archaic
- Verneuil's disease – recognizing the surgeon whose name is most often associated with the disorder as a result of his 1854–1865 studies[89]
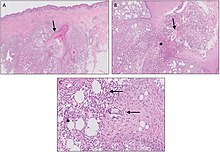
Histology
[edit]| Author | Year | Major Features |
|---|---|---|
| Plewig & Steger[85] | 1989 | Initial hyperkeratosis of the follicular infundibulum. Bacterial super-infection and follicle rupture. Granulomatous inflammatory reaction of the connective tissue. Apocrine and eccrine sweat glands secondarily involved. |
| Yu & Cook[90] | 1990 | Cysts and sinus tracts lined with epithelium, in part with hair shafts. Inflammation of apocrine sweat glands only if eccrine sweat glands and hair follicles are also inflamed. |
| Boer & Weltevreden[91] | 1996 | Primary inflammation of the follicular infundibulum. Apocrine sweat glands are secondarily involved. |
Society and culture
[edit]Experiences of people with HS
[edit]HS can have a strong negative impact on people's lives, as well as physical and mental health. People with HS often feel stigmatised and embarrassed by their condition. Many try to hide the symptoms which can lead to impaired relationships and social isolation. A multidisciplinary approach by healthcare professionals, social support networks and psychological interventions can contribute to a better quality of life.[37][38] Compared to other skin diseases, HS has one of the highest Dermatology Life Quality Index (DLQI) scores.[92]
References
[edit]- ^ a b c d e f g h i "Hidradenitis Suppurativa". NORD (National Organization for Rare Disorders). 2012. Archived from the original on 19 February 2017. Retrieved 26 October 2017.
- ^ a b c d e f g h i j k l m n o p q Jemec GB (January 2012). "Clinical practice. Hidradenitis suppurativa". The New England Journal of Medicine. 366 (2): 158–64. doi:10.1056/NEJMcp1014163. PMID 22236226.
- ^ a b c d e f g h i j k l m n "Hidradenitis suppurativa". Genetics Home Reference. December 2013. Archived from the original on 5 September 2017. Retrieved 27 October 2017.
- ^ a b c d e f "Hidradenitis suppurativa". rarediseases.info.nih.gov. 2017. Archived from the original on 28 July 2017. Retrieved 27 October 2017.
- ^ "Intergluteal contour deformity in hidradenitis suppurativa". Retrieved 18 May 2021.
- ^ Nazzaro G, Passoni E, Calzari P, Barbareschi M, Muratori S, Veraldi S, et al. (2019). "Color Doppler as a tool for correlating vascularization and pain in hidradenitis suppurativa lesions". Skin Research and Technology. 25 (6): 830–834. doi:10.1111/srt.12729. PMID 31140660. S2CID 169036038. Retrieved 18 May 2021.
- ^ Loh TY, Hendricks AJ, Hsiao JL, Shi VY (2021). "Undergarment and fabric selection in the management of hidradenitis suppurativa". Dermatology. 237 (1): 119–124. doi:10.1159/000501611. PMID 31466052. S2CID 201672889. Retrieved 18 May 2021.
- ^ Jemec G, Heidenheim M, Nielsen N (1996). "Hidradenitis suppurativa-characteristics and consequences". Clinical and Experimental Dermatology. 21 (6): 419–423. doi:10.1111/j.1365-2230.1996.tb00145.x. PMID 9167336. S2CID 25491238. Retrieved 18 May 2021.
- ^ "Psychosocial impact of hidradenitis suppurativa: a qualitative study". Retrieved 18 May 2021.
- ^ See section "Genetic Changes"[3]
- ^ a b c Pathophysiology of hidradenitis suppurativa (Seminal paper, SCMS Journal); NIH, National Library of Medicine, NCBI; 2017 Jun, 36(2):47–54.
- ^ Jemec G, Revuz J, Leyden JJ (2006). Hidradenitis Suppurativa. Springer Science & Business Media. p. 5. ISBN 978-3-540-33101-8. Archived from the original on 28 October 2017.
- ^ Dessinioti C, Katsambas A, Antoniou C (May–June 2014). "Hidradenitis suppurrativa (acne inversa) as a systemic disease". Clinics in Dermatology. 32 (3): 397–408. doi:10.1016/j.clindermatol.2013.11.006. PMID 24767187.
- ^ See section "Genetic Changes"[3]
- ^ a b Medline Plus (2012). "Hidradenitis suppurativa". U.S. National Library of Medicine. Archived from the original on 16 September 2012. Retrieved 19 September 2012.
- ^ Hopkins Medicine Staff (2024). "Inflamed/Infected Sweat Glands (Hidradenitis)". Johns Hopkins Medicine. Retrieved 27 March 2024.
- ^ a b Schawartz's principles of surgery, 8th edition, self assessment and board review, chapter 15, the skin and subcutaneous tissue, question 16
- ^ Mayo Clinic Staff (2012). "Definition". Mayo Clinic. Archived from the original on 10 September 2012. Retrieved 19 September 2012.
- ^ a b DermNet acne/hidradenitis-suppurativa
- ^ "HSF – What is Hidradenitis Suppurativa? What is HS?". Archived from the original on 6 July 2007. Retrieved 8 July 2007.
- ^ a b Slade DE, Powell BW, Mortimer PS (July 2003). "Hidradenitis suppurativa: pathogenesis and management". British Journal of Plastic Surgery. 56 (5): 451–61. doi:10.1016/S0007-1226(03)00177-2. PMID 12890458.
- ^ a b Jemec GBE. Body weight in hidradenitis suppurativa. In: Marks R, Plewig G, editors. Acne and Related disorders. London: Martin Dunitz; 1989. pp. 375–6.
- ^ König A, Lehmann C, Rompel R, Happle R (1999). "Cigarette smoking as a triggering factor of hidradenitis suppurativa". Dermatology. 198 (3): 261–4. doi:10.1159/000018126. PMID 10393449. S2CID 25343489.
- ^ Morgan WP, Hughes LE (December 1979). "The distribution, size and density of the apocrine glands in hidradenitis suppuritiva". The British Journal of Surgery. 66 (12): 853–6. doi:10.1002/bjs.1800661206. PMID 509057. S2CID 46448517.
- ^ Stellon AJ, Wakeling M (January 1989). "Hidradenitis suppurativa associated with use of oral contraceptives". BMJ. 298 (6665): 28–9. doi:10.1136/bmj.298.6665.28. PMC 1835363. PMID 2492847.
- ^ Acharya P, Mathur M (April 2020). "Hidradenitis suppurativa and smoking: A systematic review and meta-analysis". Journal of the American Academy of Dermatology. 82 (4): 1006–1011. doi:10.1016/j.jaad.2019.10.044. PMID 31678467. S2CID 207889793.
- ^ a b Scala E, Cacciapuoti S, Garzorz-Stark N, Megna M, Marasca C, Seiringer P, et al. (15 August 2021). "Hidradenitis Suppurativa: Where We Are and Where We Are Going". Cells. 10 (8): 2094. doi:10.3390/cells10082094. PMC 8392140. PMID 34440863.
- ^ Gupta AK, Knowles SR, Gupta MA, Jaunkalns R, Shear NH (February 1995). "Lithium therapy associated with hidradenitis suppurativa: case report and a review of the dermatologic side effects of lithium". Journal of the American Academy of Dermatology. 32 (2 Pt 2): 382–6. doi:10.1016/0190-9622(95)90410-7. PMID 7829746.
- ^ Hidradenitis Suppurativa at eMedicine
- ^ Von Der Werth JM, Williams HC, Raeburn JA (May 2000). "The clinical genetics of hidradenitis suppurativa revisited". The British Journal of Dermatology. 142 (5): 947–53. doi:10.1046/j.1365-2133.2000.03476.x. PMID 10809853. S2CID 35601570.
- ^ Barth JH, Kealey T (October 1991). "Androgen metabolism by isolated human axillary apocrine glands in hidradenitis suppurativa". The British Journal of Dermatology. 125 (4): 304–8. doi:10.1111/j.1365-2133.1991.tb14162.x. PMID 1954117. S2CID 34410437.
- ^ a b c Abu Rached N, Gambichler T, Ocker L, Dietrich JW, Quast DR, Sieger C, et al. (1 April 2023). "Screening for Diabetes Mellitus in Patients with Hidradenitis Suppurativa—A Monocentric Study in Germany". International Journal of Molecular Sciences. 24 (7): 6596. doi:10.3390/ijms24076596. ISSN 1422-0067. PMC 10094965. PMID 37047569.
- ^ Reference GH. "hidradenitis suppurativa". Genetics Home Reference. Archived from the original on 5 September 2017. Retrieved 5 September 2017.
- ^ Lam SY, Radjabzadeh D, Eppinga H, Nossent YR, van der Zee HH, Kraaij R, et al. (March 2021). "A microbiome study to explore the gut-skin axis in hidradenitis suppurativa". Journal of Dermatological Science. 101 (3): 218–220. doi:10.1016/j.jdermsci.2020.12.008. PMID 33423845. S2CID 231576248.
- ^ "Precocious Puberty More Common in Children with Hidradenitis Suppurativa". HCP Live. 23 September 2024. Retrieved 28 September 2024.
- ^ Mastacouris N, Midgette B, Strunk A, Garg A (18 September 2024). "Precocious Puberty Among Children and Adolescents With Hidradenitis Suppurativa". JAMA Dermatology. 160 (11): 1245. doi:10.1001/jamadermatol.2024.3104. ISSN 2168-6068. PMID 39292442.
- ^ a b c "People with the skin condition, hidradenitis suppurativa, need earlier diagnoses, more treatment options and wider support". NIHR Evidence (Plain English summary). National Institute for Health and Care Research. 1 February 2022. doi:10.3310/alert_48917. S2CID 246548949.
- ^ a b c Howells L, Lancaster N, McPhee M, Bundy C, Ingram J, Leighton P, et al. (29 May 2021). "Thematic synthesis of the experiences of people with hidradenitis suppurativa: a systematic review*". British Journal of Dermatology. 185 (5): 921–934. doi:10.1111/bjd.20523. ISSN 0007-0963. PMID 34050935. S2CID 235242411.
- ^ Saunte D, Boer J, Stratigos A, Szepietowski J, Hamzavi I, Kim K, et al. (21 July 2015). "Diagnostic delay in hidradenitis suppurativa is a global problem". British Journal of Dermatology. 173 (6): 1546–1549. doi:10.1111/bjd.14038. PMID 26198191. S2CID 41589200.
- ^ Giang J, Seelen MA, van Doorn MB, Rissmann R, Prens EP, Damman J (2018). "Complement Activation in Inflammatory Skin Diseases". Frontiers in Immunology. 9: 639. doi:10.3389/fimmu.2018.00639. ISSN 1664-3224. PMC 5911619. PMID 29713318.
- ^ a b "HS-USA :: What is Hidradenitis Suppurativa?". Archived from the original on 17 June 2013. Retrieved 20 July 2013.
- ^ Hurley HJ. Axillary hyperhidrosis, apocrine bromhidrosis, hidradenitis suppurativa, and familial benign pemphigus: surgical approach. In: Roenigk RK, Roenigk HH, editors. Dermatologic surgery. Marcel Dekker, New York, 1989, pp. 729–739.
- ^ Sartorius K, Lapins J, Emtestam L, Jemec GB (July 2003). "Suggestions for uniform outcome variables when reporting treatment effects in hidradenitis suppurativa". The British Journal of Dermatology. 149 (1): 211–3. doi:10.1046/j.1365-2133.2003.05390.x. PMID 12890229. S2CID 46142606.
- ^ Wolkenstein P, Loundou A, Barrau K, Auquier P, Revuz J (April 2007). "Quality of life impairment in hidradenitis suppurativa: a study of 61 cases". Journal of the American Academy of Dermatology. 56 (4): 621–3. doi:10.1016/j.jaad.2006.08.061. PMID 17097366.
- ^ Ingram JR, Woo PN, Chua SL, Ormerod AD, Desai N, Kai AC, et al. (May 2016). "Interventions for hidradenitis suppurativa: a Cochrane systematic review incorporating GRADE assessment of evidence quality". The British Journal of Dermatology. 174 (5): 970–8. doi:10.1111/bjd.14418. PMC 5021164. PMID 26801356.
- ^ Sharma R (1 June 2023). "Novartis Cosentyx gets European Commission nod for use in adults with hidradenitis suppurativa". medicaldialogues.in. Retrieved 1 June 2023.
- ^ Dell'Antonia M, Anedda J, Tatti A, Falco A, Sanna S, Ferreli C, et al. (April 2023). "Non-surgical treatment of hidradenitis suppurativa: the role of cryotherapy". Frontiers in Medicine. 10. doi:10.3389/fmed.2023.1141691. PMC 10151524. PMID 37144039.
- ^ Scheinfeld N (April 2013). "Hidradenitis suppurativa: A practical review of possible medical treatments based on over 350 hidradenitis patients". Dermatology Online Journal. 19 (4): 1. doi:10.5070/D35VW402NF. PMID 24021361.
- ^ Clemmensen OJ (June 1983). "Topical treatment of hidradenitis suppurativa with clindamycin". International Journal of Dermatology. 22 (5): 325–8. doi:10.1111/j.1365-4362.1983.tb02150.x. PMID 6347922. S2CID 46661288.
- ^ {{Nosrati A, Ch'en PY, Torpey ME, Shokrian N, Ball G, Benesh G, Andriano TM, Zhu TR, Heibel HD, Hosgood HD, Campton KL, Cohen SR. Efficacy and Durability of Intravenous Ertapenem Therapy for Recalcitrant Hidradenitis Suppurativa. JAMA Dermatol. 2024 Feb 14:e236201. doi: 10.1001/jamadermatol.2023.6201. Epub ahead of print. PMID 38353987; PMCID: PMC10867774.}}
- ^ a b Nikolakis G, Kyrgidis A, Zouboulis CC (2019). "Is There a Role for Antiandrogen Therapy for Hidradenitis Suppurativa? A Systematic Review of Published Data". American Journal of Clinical Dermatology. 20 (4): 503–513. doi:10.1007/s40257-019-00442-w. ISSN 1175-0561. PMID 31073704. S2CID 149443722.
- ^ a b Goldburg SR, Strober BE, Payette MJ (2019). "Part 2. Current and emerging treatments for hidradenitis suppurativa". Journal of the American Academy of Dermatology. 82 (5): 1061–1082. doi:10.1016/j.jaad.2019.08.089. ISSN 0190-9622. PMID 31604100. S2CID 204331143.
- ^ Student S, Hejmo T, Poterała-Hejmo A, Leśniak A, Bułdak R (2020). "Anti-androgen hormonal therapy for cancer and other diseases". European Journal of Pharmacology. 866: 172783. doi:10.1016/j.ejphar.2019.172783. ISSN 0014-2999. PMID 31712062.
- ^ Cusack C, Buckley C (April 2006). "Etanercept: effective in the management of hidradenitis suppurativa". The British Journal of Dermatology. 154 (4): 726–9. doi:10.1111/j.1365-2133.2005.07067.x. PMID 16536817. S2CID 23743987.
- ^ Haslund P, Lee RA, Jemec GB (November 2009). "Treatment of hidradenitis suppurativa with tumour necrosis factor-alpha inhibitors". Acta Dermato-Venereologica. 89 (6): 595–600. doi:10.2340/00015555-0747. PMID 19997689.
- ^ Ingram JR (May 2017). "Interventions for Hidradenitis Suppurativa: Updated Summary of an Original Cochrane Review". JAMA Dermatology. 153 (5): 458–459. doi:10.1001/jamadermatol.2017.0432. PMID 28355440.
- ^ "FDA approves Novartis Cosentyx® as the first new biologic treatment option for hidradenitis suppurativa patients in nearly a decade".
- ^ "HS Signs and Symptoms | COSENTYX® (Secukinumab)".
- ^ Nickle SB, Peterson N, Peterson M (April 2014). "Updated Physician's Guide to the Off-label Uses of Oral Isotretinoin". The Journal of Clinical and Aesthetic Dermatology. 7 (4): 22–34. PMC 3990537. PMID 24765227.
- ^ Molinelli E, Brisigotti V, Campanati A, Sapigni C, Giacchetti A, Cota C, et al. (August 2020). "Efficacy of oral zinc and nicotinamide as maintenance therapy for mild/moderate hidradenitis suppurativa: A controlled retrospective clinical study". Journal of the American Academy of Dermatology. 83 (2): 665–667. doi:10.1016/j.jaad.2020.04.092. PMID 32339699.
- ^ Blok J, Spoo J, Leeman F, Jonkman M, Horváth B (February 2015). "Skin-Tissue-sparing Excision with Electrosurgical Peeling (STEEP): a surgical treatment option for severe hidradenitis suppurativa Hurley stage II/III". Journal of the European Academy of Dermatology and Venereology. 29 (2): 379–382. doi:10.1111/jdv.12376. PMID 24460855. S2CID 21974148.
- ^ Scheinfeld N (April 2013). "Hidradenitis suppurativa: A practical review of possible medical treatments based on over 350 hidradenitis patients". Dermatology Online Journal. 19 (4): 1. doi:10.5070/D35VW402NF. PMID 24021361. Archived from the original on 6 March 2014. Retrieved 4 March 2014.
- ^ Xu LY, Wright DR, Mahmoud BH, Ozog DM, Mehregan DA, Hamzavi IH (January 2011). "Histopathologic study of hidradenitis suppurativa following long-pulsed 1064-nm Nd:YAG laser treatment". Archives of Dermatology. 147 (1): 21–8. doi:10.1001/archdermatol.2010.245. PMID 20855672.
- ^ Ravi M, Trinidad J (2022). "Botulinum Toxin in Hidradenitis Suppurativa: A Systematic Review". Journal of Drugs in Dermatology : JDD. 21 (4): 408–412. PMID 35389587.
- ^ Talmant JC, Bruant-Rodier C, Nunziata AC, Rodier JF, Wilk A (February 2006). "[Squamous cell carcinoma arising in Verneuil's disease: two cases and literature review]". Annales de Chirurgie Plastique et Esthétique (in French). 51 (1): 82–6. doi:10.1016/j.anplas.2005.11.002. PMID 16488526.
- ^ Short KA, Kalu G, Mortimer PS, Higgins EM (September 2005). "Vulval squamous cell carcinoma arising in chronic hidradenitis suppurativa". Clinical and Experimental Dermatology. 30 (5): 481–3. doi:10.1111/j.1365-2230.2005.01875.x. PMID 16045671. S2CID 33438993.
- ^ a b Abu Rached N, Dietrich JW, Ocker L, Quast DR, Stockfleth E, Bechara FG (6 August 2024). "Diabetes remission associated with optimized treatment of hidradenitis suppurativa". Journal der Deutschen Dermatologischen Gesellschaft = Journal of the German Society of Dermatology. 22 (10): 1427–1429. doi:10.1111/ddg.15490. PMID 39106221.
- ^ Hurley HJJ. Apocrine glands. New York: McGraw Hill; 1979.
- ^ Tennant F, Bergeron JR, Stone OJ, Mullins JF (August 1968). "Anemia associated with hidradenitis suppurativa". Archives of Dermatology. 98 (2): 138–40. doi:10.1001/archderm.98.2.138. PMID 5667225.
- ^ Schneeweiss MC, Kim SC, Schneeweiss S, Rosmarin D, Merola JF (2020). "Risk of inflammatory arthritis after a new diagnosis of hidradenitis suppurativa". JAMA Dermatology. 156 (3): 342–345. doi:10.1001/jamadermatol.2019.4590. PMC 6990727. PMID 31968066.
- ^ Williams ST, Busby RC, DeMuth RJ, Nelson H (May 1991). "Perineal hidradenitis suppurativa: presentation of two unusual complications and a review". Annals of Plastic Surgery. 26 (5): 456–62. doi:10.1097/00000637-199105000-00008. PMID 1952719.
- ^ Lapins J, Ye W, Nyrén O, Emtestam L (June 2001). "Incidence of cancer among patients with hidradenitis suppurativa". Archives of Dermatology. 137 (6): 730–4. PMID 11405761.
- ^ Moschella SL (October 1966). "Hidradenitis suppurativa. Complications resulting in death". JAMA. 198 (1): 201–3. doi:10.1001/jama.198.1.201. PMID 5953172.
- ^ Vasey FB, Fenske NA, Clement GB, Bridgeford PH, Germain BF, Espinoza LR (1984). "Immunological studies of the arthritis of acne conglobata and hidradenitis suppurativa". Clinical and Experimental Rheumatology. 2 (4): 309–11. PMID 6241861.
- ^ Jalenques I, Ciortianu L, Pereira B, D'Incan M, Lauron S, Rondepierre F (25 March 2020). "The prevalence and odds of anxiety and depression in children and adults with hidradenitis suppurativa: Systematic review and meta-analysis". Journal of the American Academy of Dermatology. 83 (2): 542–553. doi:10.1016/j.jaad.2020.03.041. PMID 32222447. S2CID 214716227.
- ^ a b c d Ingram JR (3 September 2020). "The epidemiology of hidradenitis suppurativa*". British Journal of Dermatology. 183 (6): 990–998. doi:10.1111/bjd.19435. ISSN 0007-0963. PMID 32880911. S2CID 221475227.
- ^ Abu Rached N, Gambichler T, Dietrich JW, Ocker L, Seifert C, Stockfleth E, et al. (3 December 2022). "The Role of Hormones in Hidradenitis Suppurativa: A Systematic Review". International Journal of Molecular Sciences. 23 (23): 15250. doi:10.3390/ijms232315250. PMC 9736970. PMID 36499573.
- ^ Abu Rached N, Dietrich JW, Ocker L, Quast DR, Scheel C, Gambichler T, et al. (4 December 2023). "Primary Thyroid Dysfunction Is Prevalent in Hidradenitis Suppurativa and Marked by a Signature of Hypothyroid Graves' Disease: A Case-Control Study". Journal of Clinical Medicine. 12 (23): 7490. doi:10.3390/jcm12237490. PMC 10707714. PMID 38068542.
- ^ Velpeau A. Aissele. In: Bechet Jeune Z: Dictionnaire de médecine, on Repertoire Générale des Sciences Medicals sous le Rapport Theorique et Pratique. 1839.
- ^ Verneuil AS (1854). "Etudes sur les tumeurs de la peau et quelques maladies de glandes sudoripares" [Studies on skin tumors; some diseases of the sweat glands]. Archives of General Medicine (in French). 94: 693–705.
- ^ Schiefferdecker B (1922). Die Hautdrüsen der Menschen und der Säugetiere, ihre histologische und rassenanatomische Bedeutung sowie die muscularis sexualis [The skin glands of humans and mammals, their histological and anatomical racial meaning and muscularis sexualis]. Stuttgart: Schweizerbart E.[page needed]
- ^ Pillsbury DM, Shelley WB, Kligmann AM (1956). "Bacterial infections of the skin". In Pillsbury DM (ed.). Dermatoloy (1st ed.). Philadelphia. pp. 482–9.
{{cite book}}: CS1 maint: location missing publisher (link) - ^ Triads in Dermatology; Prachi G Agrawal, Uday S Khopkar, [...], and Sunil N Mishra; Indian J Dermatol. 2013 Sep–Oct; 58(5): 346–351
- ^ Plewig G, Kligman AM (1975). "Acne Conglobata". In Plewig G, Kligman AM (eds.). Acne. pp. 168–203. doi:10.1007/978-3-642-96246-2_11. ISBN 978-3-642-96246-2.
- ^ a b Plewig G, Steger M (1989). "Acne inversa (alias acne triad, acne tetrad or hidradenitis suppurativa)". In Marks R, Plewig G (eds.). Acne and Related Disorders. London: Martin Dunitz. pp. 345–57.
- ^ Sellheyer K, Krahl D (July 2005). ""Hidradenitis suppurativa" is acne inversa! An appeal to (finally) abandon a misnomer". International Journal of Dermatology. 44 (7): 535–40. doi:10.1111/j.1365-4632.2004.02536.x. PMID 15985019. S2CID 34144101.
- ^ Bazex J, Bayle P, San B (March 2007). "Hidradenitis suppurativa is acne inversa". International Journal of Dermatology. 46 (3): 330, author reply 330–2. doi:10.1111/j.1365-4632.2007.02872.x. PMID 17343599. S2CID 43108078.
- ^ Scheinfeld N (December 2006). "Hidradenitis should not be renamed acne inversa". Dermatology Online Journal. 12 (7): 6. doi:10.5070/D35G21T4MQ. PMID 17459292.
- ^ Verneuil AS (1854). "Etudes sur les tumor de la peau". Arch Gen Med (in French). 94: 693.
- ^ Yu CC, Cook MG (June 1990). "Hidradenitis suppurativa: a disease of follicular epithelium, rather than apocrine glands". The British Journal of Dermatology. 122 (6): 763–9. doi:10.1111/j.1365-2133.1990.tb06264.x. PMID 2369556. S2CID 8857181.
- ^ Boer J, Weltevreden EF (November 1996). "Hidradenitis suppurativa or acne inversa. A clinicopathological study of early lesions". The British Journal of Dermatology. 135 (5): 721–5. doi:10.1111/j.1365-2133.1996.tb03880.x (inactive 27 November 2024). PMID 8977671.
{{cite journal}}: CS1 maint: DOI inactive as of November 2024 (link) - ^ van Straalen KR, Prens EP, Gudjonsson JE (April 2022). "Insights into hidradenitis suppurativa". The Journal of Allergy and Clinical Immunology. 149 (4): 1150–1161. doi:10.1016/j.jaci.2022.02.003. PMID 35189127. S2CID 247006893.
External links
[edit]- Hidradenitis suppurativa at American Academy of Dermatology Association
- Hidradenitis suppurativa at British Association of Dermatologists
- Hidradenitis Suppurativa Foundation
