Tennis elbow
| Tennis elbow | |
|---|---|
| Other names | Lateral epicondylitis, lateral elbow tendinopathy[1] |
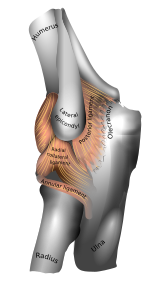 | |
| Left elbow-joint. (Lateral epicondyle visible at center.) | |
| Specialty | Orthopedics, sports medicine |
| Symptoms | Painful and tender outer part of the elbow[1] |
| Usual onset | Gradual[2] |
| Duration | Less than 1 to 2 years[3] |
| Causes | Middle age (ages 35-60). |
| Diagnostic method | Symptoms and physical examination |
| Differential diagnosis | Osteoarthritis |
| Treatment | Nothing is proved to alter the natural course of the disease. Exercises, braces, ice or heat, and medications may be palliative. |
Tennis elbow, also known as lateral epicondylitis or enthesopathy of the extensor carpi radialis origin, is an enthesopathy (attachment point disease) of the origin of the extensor carpi radialis brevis on the lateral epicondyle.[1][4] Those with tennis elbow often report pain and tenderness over the bony prominence of the lateral epicondyle, which serves as the common origin of the forearm and hand’s long extensor tendons. Symptoms range from mild tenderness to severe, persistent pain.[1][5][6] The pain may also extend into the back of the forearm.[2] Onset of symptoms is generally gradual, although they can seem sudden and be misinterpreted as an injury.[7][2][8]
Tennis elbow is generally considered idiopathic, with the exact cause and pathogenesis still unknown, though it is thought to involve tendinosis, a degenerative process of the local tendon.[9][10]
It is often stated that the condition is caused by excessive use of the muscles of the back of the forearm, but this is not supported by experimental evidence and is a common misinterpretation or unhelpful thought about symptoms.[11][2][12] It may be associated with work or sports, classically racquet sports (including paddle sports), but most people with the condition are not exposed to these activities.[1][2][13] The diagnosis is based on the symptoms and examination. Medical imaging is not particularly useful.[2][10] Signs consistent with the diagnosis include pain when a subject tries to bend back the wrist against resistance.[1]
The natural history of untreated enthesopathy is resolution over a period of 1–2 years.[14] Palliative (symptoms alleviating) treatment may include pain medications such as NSAIDS or acetaminophen (paracetamol), a wrist brace, or a strap over the upper forearm.[1][2] The role of corticosteroid injections as a form of treatment is still debated.[15] Recent evidence suggests that corticosteroid injections may delay symptom resolution.[16]
Signs and symptoms
[edit]Patients typically experience pain or burning around the outer part of the elbow (lateral epicondyle of the humerus), which can radiate down the forearm and sometimes up to the upper arm. The pain is often triggered or worsened by activities that involve resisted wrist extension, such as gripping objects.[17][18] Pain intensity varies from mild to severe and can be intermittent or constant, significantly impacting daily life. Patients also commonly report grip weakness and difficulty lifting.[19]
Terminology
[edit]The term "tennis elbow" is widely used (although informal), but the condition should be understood as not limited to tennis players.[20][21] Historically, the medical term "lateral epicondylitis" was most commonly used for the condition, but "itis" implies inflammation and the condition is not inflammatory.[2][20][21][22][23]
Since histological findings reveal noninflammatory tissue, the terms "lateral elbow tendinopathy" and "tendinosis" are suggested.[24][25] In 2019, a group of international experts suggested that "lateral elbow tendinopathy" was the most appropriate terminology.[26] But a disease of an attachment point (or enthesia) is most accurately referred to as an "enthesopathy."[27]
Causes
[edit]
The exact cause of lateral epicondylitis remains unclear. However, it is often linked to repetitive microtrauma resulting from excessive gripping, wrist extension, radial deviation, and/or forearm supination.[28][29]
Traditionally, people have speculated that tennis elbow is a type of repetitive strain injury resulting from tendon overuse and failed healing of the tendon, but there is no evidence of injury or repair on histopathology, and misinterpretation of painful activities as a source of damage is common.[30]

Pathophysiology
[edit]The extensor carpi radialis brevis is the most commonly affected muscle in lateral epicondylitis (LE), along with other extensor carpal muscles. Due to its unique origin, the ECRB tendon is prone to abrasion during elbow movements, leading to repetitive microtrauma.
Lateral epicondylitis was Initially considered an inflammatory process, however there is no evidence of inflammation or repair.[23] Therefore, the disorder is more appropriately referred to as tendinosis or tendinopopathy.[24] Tendinosis, a degenerative condition with fibroblasts, abnormal collagen, and increased blood vessels. Repetitive stress causes microtears, scar tissue formation, and biomechanical changes, worsening symptoms over time.
Clinical evalulation
[edit]Physical examination
[edit]Diagnosis is based on symptoms and clinical signs that are discrete and characteristic. For example, the extension of the elbow and flexion of the wrist causes outer elbow pain. The physical examination usually reveals marked tenderness at the origin of the extensor carpi radialis brevis muscle from the lateral epicondyle (extensor carpi radialis brevis origin).[31] Pain may worsen with resisted wrist extension, middle finger extension, and forearm supination with an extended elbow, although normal elbow movement is often maintained, even in severe cases.[18]
Cozen's test
[edit]Cozen's test is a physical examination performed to evaluate for tennis elbow involving pain with resisted wrist extension.[32] The test is said to be positive if a resisted wrist extension triggers pain to the lateral aspect of the elbow owing to stress placed upon the tendon of the extensor carpi radialis brevis muscle.[33] The test is performed with extended elbow. NOTE: With elbow flexed the extensor carpi radialis longus is in a shortened position as its origin is the lateral supracondylar ridge of the humerus. To rule out the ECRB (extensor carpi radialis brevis), repeat the test with the elbow in full extension.
Medical imaging
[edit]Medical imaging is not necessary or helpful.[34]
Radiographs (X-rays) may demonstrate calcification where the extensor muscles attach to the lateral epicondyle.[31] Medical ultrasonography and magnetic resonance imaging (MRI) can demonstrate the pathology, but are not helpful for diagnosis and do not influence treatment.[35][36]
Longitudinal sonogram of the lateral elbow displays thickening and heterogeneity of the common extensor tendon that is consistent with tendinosis, as the ultrasound reveals calcifications, intrasubstance tears, and marked irregularity of the lateral epicondyle. Although the term “epicondylitis” is frequently used to describe this disorder, most histopathologic findings of studies have displayed no evidence of an acute, or a chronic inflammatory process. Histologic studies have demonstrated that this condition is the result of tendon degeneration, which replaces normal tissue with a disorganized arrangement of collagen. Colour Doppler ultrasound reveals structural tendon changes, with vascularity and hypo-echoic areas that correspond to the areas of pain in the extensor origin.[37]
Table of Clinical classification of lateral epicondylitis phases.[38]
| Phase | Description of pain changes at differnet phases |
|---|---|
| I | Mild pain after activity, usually recovers within 24 hours |
| II | Mild pain more than 48 hours after activity, no pain during activity, can be relieved with warm-up exercises, and recovers within 72 hours |
| III | Mild pain before and during activity, no significant negative impact on the activities, and can be partially relieved with warm-up exercises |
| IV | Mild pain accompanies the activities of daily living and has negative impact on the performance of activities |
| V | Harmful pain unrelated to activities, great negative impact on the performance of activities but does not prevent the activities of daily life. Need complete rest to control the pain |
| VI | Persistent pain despite complete rest and can prevent the activities of daily life |
| VII | Consistent pain at rest, aggravated after activities, and disturbed sleep |
Treatment
[edit]Despite advances in the treatment of LE, there is still a lack of established standards. It is generally self-limiting, and most cases require no treatment, with up to 80% cases recovering within one year.[39] Patients with prolonged symptoms may require further conservative or surgical treatments. Palliative (symptoms alleviating) treatment may include pain medications such as NSAIDS or acetaminophen (paracetamol), a wrist brace, or a strap over the upper forearm.[1][40]
Exercises
[edit]Stretching and isometric strengthening are the most common recommended exercises.
The muscle is stretched with the elbow straight and the wrist passively flexed.
Isometric strengthening can be done by pushing the top of the hand up against the undersurface of a table and holding the wrist straight.[41]
Orthotic devices
[edit]

Orthosis is a device externally used on the limb to improve the function or reduce the pain. Orthotics may be useful in tennis elbow; however, long-term effects are unknown.[42] There are two main types of orthoses prescribed for this problem: counterforce elbow orthoses and wrist extension orthoses. Counterforce orthosis has a circumferential structure surrounding the arm. This orthosis usually has a strap which applies a binding force over the origin of the wrist extensors. The applied force by orthosis reduces the elongation within the musculotendinous fibers. Wrist extensor orthosis maintains the wrist in the slight extension.
Speculative treatments
[edit]Other approaches that are not experimentally tested include eccentric exercise using a rubber bar, joint manipulation directed at the elbow and wrist, spinal manipulation directed at the cervical and thoracic spinal regions, low level laser therapy, and extracorporeal shockwave therapy.[43][44][45][46][47]
Medication
[edit]Although anti-inflammatories are a commonly prescribed treatment for tennis elbow, the evidence for their effect is usually anecdotal with only limited studies showing a benefit.[48] A systematic review found that topical non-steroidal anti-inflammatory drugs (NSAIDs) may improve pain in the short term (up to 4 weeks) but was unable to draw firm conclusions due to methodological issues.[49] Evidence for oral NSAIDs is mixed.[49]
Evidence is poor for long term improvement from injections of any type, whether corticosteroids, botulinum toxin, prolotherapy, or other substances.[50] Corticosteroid injection may be effective in the short term;[51] however, they are of little benefit after a year, compared to a wait-and-see approach.[52] A randomized control trial comparing the effect of corticosteroid injection, physiotherapy, or a combination of corticosteroid injection and physiotherapy found that patients treated with corticosteroid injection versus placebo had lower complete recovery or improvement at 1 year (Relative risk 0.86). Patients that received corticosteroid injection also had a higher recurrence rate at 1 year versus placebo (54% versus 12%, relative risk 0.23).[53] Complications from repeated steroid injections include skin problems such as hypopigmentation and fat atrophy leading to indentation of the skin around the injection site.[51] Steroid injections appear to be more effective than shock wave therapy.[54] Botulinum toxin type A to paralyze the forearm extensor muscles in those with chronic tennis elbow that has not improved with conservative measures may be viable.[55]
Surgery
[edit]Surgery is an option.[56][57][58] Surgical methods include:[59]
- Lengthening, release, debridement, or repair of the origin of the extrinsic extensor muscles of the hand at the lateral epicondyle
Surgical techniques for lateral epicondylitis can be done by open surgery, percutaneous surgery, or arthroscopic surgery, with no high-quality evidence that any particular type is better or worse than another.[60][57] Side effects include infection, damage to nerves, and inability to straighten the arm.[61] A review of the evidence related to surgery found that published studies were of low quality and did not show that surgery was any more effective than other treatments.[60] A subsequent research trial showed that surgery was no more effective than sham surgery, where patients only received a skin incision, although the trial was limited by a small number of patients.[62]
Epidemiology
[edit]Enthesopathy of the ECRB origin
[edit]Evidence from imaging studies suggests that about 1 in 5 humans have detectable enthesopathy of the extensor carpi radialis brevis origin in their lifetime.[63] Symptoms likely vary and are self-limited. The signal changes on MRI seem permanent. There is no evidence that specific occupations or activities are associated with enthesopathy.[64]
Symptoms of lateral epicondylitis
[edit]Symptoms suggestive of lateral epicondylitis are present in about 1% of the adult population and are most common between ages 40 and 60.[64] The prevalence varies somewhat between studies, likely as a result of varied diagnostic criteria and limited reliability between different observers.[64] The data regarding symptoms of lateral epicondylitis in relation to occupations and sports are inconsistent and inconclusive.[64] The shortcomings of the evidence that addresses the relationship between symptoms and occupation/sport include: variation in diagnostic criteria, limited reliability of diagnosis, confounding association of psychosocial factors, selection bias due to a high non-response rate, and the fact that exposures are usually by subjective patient reports and symptomatic patients might receive greater exposure.
History
[edit]German physician F. Runge[65] is usually credited for the first description of the condition, calling it as "writer's cramp" (Schreibekrampf) in 1873.[66] Later, it was called as "washer women's elbow".[67] British surgeon Henry Morris published an article in The Lancet describing "lawn tennis arm" in 1883.[68][65] The popular term "tennis elbow" first appeared the same year in a paper by H. P. Major, described as "lawn-tennis elbow".[69][70]
See also
[edit]References
[edit]- ^ a b c d e f g h Hubbard MJ, Hildebrand BA, Battafarano MM, Battafarano DF (June 2018). "Common Soft Tissue Musculoskeletal Pain Disorders". Primary Care. 45 (2): 289–303. doi:10.1016/j.pop.2018.02.006. PMID 29759125. S2CID 46886582.
- ^ a b c d e f g h "Tennis Elbow (Lateral Epicondylitis)". OrthoInfo. July 2015. Retrieved 21 June 2018.
- ^ Vaquero-Picado A, Barco R, Antuña SA (November 2016). "Lateral epicondylitis of the elbow". EFORT Open Reviews. 1 (11): 391–397. doi:10.1302/2058-5241.1.000049. PMC 5367546. PMID 28461918.
- ^ Faro, Frances; Wolf, Jennifer Moriatis (October 2007). "Lateral Epicondylitis: Review and Current Concepts". The Journal of Hand Surgery. 32 (8): 1271–1279. doi:10.1016/j.jhsa.2007.07.019. ISSN 0363-5023.
- ^ Behazin M, Kachooei AR (March 2021). "Arthroscopic Recession Technique in the Surgery of Tennis Elbow by Sharp Cutting the Extensor Carpi Radialis Brevis (ECRB) Tendon Origin". The Archives of Bone and Joint Surgery. 9 (2): 174–179. doi:10.22038/abjs.2020.48173.2383. PMC 8121031. PMID 34026934.
- ^ Cutts, S.; Gangoo, Shafat; Modi, Nitin; Pasapula, Chandra (2020). "Tennis elbow: A clinical review article". Journal of Orthopaedics. 17: 203–207. doi:10.1016/j.jor.2019.08.005. ISSN 0972-978X. PMC 6926298. PMID 31889742.
- ^ Lemmers, M.; Versluijs, Y.; Kortlever, J.; Gonzalez, A.; Ring, D. (2020). "Misperception of Disease Onset in People with Gradual-Onset Disease of the Upper Extremity". The Journal of Bone and Joint Surgery. 102 (24): 2174–2180. doi:10.2106/JBJS.20.00420. hdl:1887/3638637. PMID 33027085. S2CID 222211926.
- ^ Solheim E, Hegna J, Øyen J (June 2011). "Extensor tendon release in tennis elbow: results and prognostic factors in 80 elbows". Knee Surgery, Sports Traumatology, Arthroscopy. 19 (6): 1023–1027. doi:10.1007/s00167-011-1477-1. PMC 3096769. PMID 21409461.
- ^ Gorski JM (August 2019). "Evaluation of Sleep Position for Possible Nightly Aggravation and Delay of Healing in Tennis Elbow". Journal of the American Academy of Orthopaedic Surgeons. Global Research & Reviews. 3 (8): e082. doi:10.5435/JAAOSGlobal-D-19-00082. PMC 6754212. PMID 31592507.
- ^ a b Ma KL, Wang HQ (2020). "Management of Lateral Epicondylitis: A Narrative Literature Review". Pain Research & Management. 2020: 6965381. doi:10.1155/2020/6965381. PMC 7222600. PMID 32454922.
- ^ Teunis, T.; Salman, A. A. I.; Koeing, K.; Ring, D.; Amirreza, A. (2022). "Unhelpful Thoughts and Distress Regarding Symptoms Limit Accommodation of Musculoskeletal Pain". Clin Orthop Relat Res. 480 (2): 276–283. doi:10.1097/corr.0000000000002006. PMC 8747479. PMID 34652286. S2CID 238990392.
- ^ Bunata RE, Brown DS, Capelo R (September 2007). "Anatomic factors related to the cause of tennis elbow". The Journal of Bone and Joint Surgery. American Volume. 89 (9): 1955–1963. doi:10.2106/JBJS.F.00727. PMID 17768192.
- ^ "Mouse Elbow - Injury Overview".
- ^ Vaquero-Picado A, Barco R, Antuña SA (November 2016). "Lateral epicondylitis of the elbow". EFORT Open Reviews. 1 (11): 391–397. doi:10.1302/2058-5241.1.000049. PMC 5367546. PMID 28461918.
- ^ Saygin D, Tabib T, Bittar HE, Valenzi E, Sembrat J, Chan SY, et al. (2022-09-06). "Transcriptional profiling of lung cell populations in idiopathic pulmonary arterial hypertension". Pulmonary Circulation. 10 (1). Wiley. doi:10.1002/14651858.cd001978.pub2. PMC 7052475. PMID 32166015. S2CID 252151420.
- ^ Hsieh LF, Kuo YC, Lee CC, Liu YF, Liu YC, Huang V (February 2018). "Comparison Between Corticosteroid and Lidocaine Injection in the Treatment of Tennis Elbow: A Randomized, Double-Blinded, Controlled Trial". American Journal of Physical Medicine & Rehabilitation. 97 (2): 83–89. doi:10.1097/PHM.0000000000000814. PMID 28816704. S2CID 24498663.
- ^ Hsu, Stephanie H.; Moen, Todd C.; Levine, William N.; Ahmad, Christopher S. (March 2012). "Physical examination of the athlete's elbow". The American Journal of Sports Medicine. 40 (3): 699–708. doi:10.1177/0363546511428869. ISSN 1552-3365. PMID 22156170.
- ^ a b Ahmad, Z.; Siddiqui, N.; Malik, S. S.; Abdus-Samee, M.; Tytherleigh-Strong, G.; Rushton, N. (March 2013). "Lateral epicondylitis: a review of pathology and management". The Bone & Joint Journal. 95-B (9): 1158–1164. doi:10.1302/0301-620X.95B9.29285. ISSN 2049-4408. PMID 23997125.
- ^ Dorf, Erik R.; Chhabra, A. Bobby; Golish, S. Raymond; McGinty, Jasmin L.; Pannunzio, Michael E. (2007). "Effect of elbow position on grip strength in the evaluation of lateral epicondylitis". The Journal of Hand Surgery. 32 (6): 882–886. doi:10.1016/j.jhsa.2007.04.010. ISSN 0363-5023. PMID 17606071.
- ^ a b "Tennis elbow (lateral epicondylitis) Elbow Pain". Cleveland Clinic. 2018. Retrieved 23 January 2018.
- ^ a b "Tennis elbow". Mayo Clinic. 2 August 2017. Retrieved 23 January 2018.
- ^ Smith C (18 June 2004). "What is tennis elbow?". BBC Sport Academy. Retrieved 23 January 2018.
- ^ a b Nirschl RP, Ashman ES (2004-01-01). "Tennis elbow tendinosis (epicondylitis)". Instructional Course Lectures. 53: 587–598. PMID 15116648.
- ^ a b McShane JM, Nazarian LN, Harwood MI (October 2006). "Sonographically guided percutaneous needle tenotomy for treatment of common extensor tendinosis in the elbow". Journal of Ultrasound in Medicine. 25 (10): 1281–1289. doi:10.7863/jum.2006.25.10.1281. PMID 16998100. S2CID 22963436.
- ^ du Toit C, Stieler M, Saunders R, Bisset L, Vicenzino B (November 2008). "Diagnostic accuracy of power Doppler ultrasound in patients with chronic tennis elbow". British Journal of Sports Medicine. 42 (11): 872–876. doi:10.1136/bjsm.2007.043901. hdl:10072/22142. PMID 18308874. S2CID 3274396.
- ^ Scott A, Squier K, Alfredson H, Bahr R, Cook JL, Coombes B, et al. (March 2020). "ICON 2019: International Scientific Tendinopathy Symposium Consensus: Clinical Terminology". British Journal of Sports Medicine. 54 (5): 260–262. doi:10.1136/bjsports-2019-100885. hdl:10397/97289. PMID 31399426. S2CID 199517946.
- ^ Ikonen J, Lähdeoja T, Ardern CL, Buchbinder R, Reito A, Karjalainen T (April 2022). "Persistent Tennis Elbow Symptoms Have Little Prognostic Value: A Systematic Review and Meta-analysis". Clinical Orthopaedics and Related Research. 480 (4): 647–660. doi:10.1097/CORR.0000000000002058. PMC 8923574. PMID 34874323.
- ^ Eygendaal, Denise; Rahussen, F. Th G.; Diercks, R. L. (November 2007). "Biomechanics of the elbow joint in tennis players and relation to pathology". British Journal of Sports Medicine. 41 (11): 820–823. doi:10.1136/bjsm.2007.038307. ISSN 1473-0480. PMC 2465285. PMID 17638843.
- ^ Lee, Han-Sung; Park, Ho Youn; Yoon, Jun O.; Kim, Jin Sam; Chun, Jae Myeung; Aminata, Iman W.; Cho, Won-Joon; Jeon, In-Ho (September 2013). "Musicians' medicine: musculoskeletal problems in string players". Clinics in Orthopedic Surgery. 5 (3): 155–160. doi:10.4055/cios.2013.5.3.155. ISSN 2005-4408. PMC 3758983. PMID 24009899.
- ^ Gunn CC, Milbrandt WE (May 1976). "Tennis elbow and the cervical spine". Canadian Medical Association Journal. 114 (9): 803–809. PMC 1957126. PMID 1268791.
- ^ a b Sarwark JF (2010). Essentials of musculoskeletal care. Rosemont, Ill.: American Academy of Orthopaedic Surgeons. ISBN 978-0892035793. OCLC 706805938.
- ^ "Tennis elbow". MedlinePlus Medical Encyclopedia.
- ^ Cooper G (2007-10-28). Pocket Guide to Musculoskeletal Diagnosis. Springer Science & Business Media. pp. 44–. ISBN 978-1-59745-009-6.
- ^ Orchard J, Kountouris A (May 2011). "The management of tennis elbow". BMJ. 342: d2687. doi:10.1136/bmj.d2687. PMID 21558359. S2CID 8358075.
- ^ Keijsers R, de Vos RJ, Kuijer PP, van den Bekerom MP, van der Woude HJ, Eygendaal D (October 2019). "Tennis elbow". Shoulder & Elbow. 11 (5): 384–392. doi:10.1177/1758573218797973. PMC 6739751. PMID 31534489.
- ^ "Tennis Elbow". Mayo Clinic Medical Information and Tools for Healthy Living – MayoClinic.com. 15 October 2008.
- ^ du Toit C, Stieler M, Saunders R, Bisset L, Vicenzino B (November 2008). "Diagnostic accuracy of power Doppler ultrasound in patients with chronic tennis elbow". British Journal of Sports Medicine. 42 (11): 872–876. doi:10.1136/bjsm.2007.043901. hdl:10072/22142. PMID 18308874. S2CID 3274396.
- ^ Nirschl, Robert P.; Ashman, Edward S. (October 2003). "Elbow tendinopathy: tennis elbow". Clinics in Sports Medicine. 22 (4): 813–836. doi:10.1016/s0278-5919(03)00051-6. ISSN 0278-5919. PMID 14560549.
- ^ Bisset, Leanne; Beller, Elaine; Jull, Gwendolen; Brooks, Peter; Darnell, Ross; Vicenzino, Bill (2006-11-04). "Mobilisation with movement and exercise, corticosteroid injection, or wait and see for tennis elbow: randomised trial". BMJ (Clinical research ed.). 333 (7575): 939. doi:10.1136/bmj.38961.584653.AE. ISSN 1756-1833. PMC 1633771. PMID 17012266.
- ^ "Tennis Elbow (Lateral Epicondylitis) - OrthoInfo - AAOS". www.orthoinfo.org. Retrieved 2022-12-24.
- ^ Santiago AO, Rios-Russo JL, Baerga L, Micheo W (2021-12-01). "Evidenced-Based Management of Tennis Elbow". Current Physical Medicine and Rehabilitation Reports. 9 (4): 186–194. doi:10.1007/s40141-021-00322-7. ISSN 2167-4833. S2CID 239460609.
- ^ Struijs PA, Smidt N, Arola H, Dijk C, Buchbinder R, Assendelft WJ (2002-01-21). "Orthotic devices for the treatment of tennis elbow". The Cochrane Database of Systematic Reviews. 2010 (1): CD001821. doi:10.1002/14651858.cd001821. PMC 8407516. PMID 11869609.
- ^ Tyler TF, Thomas GC, Nicholas SJ, McHugh MP (September 2010). "Addition of isolated wrist extensor eccentric exercise to standard treatment for chronic lateral epicondylosis: a prospective randomized trial". Journal of Shoulder and Elbow Surgery. 19 (6): 917–922. doi:10.1016/j.jse.2010.04.041. PMID 20579907.
- ^ Vicenzino B, Cleland JA, Bisset L (2007-01-01). "Joint manipulation in the management of lateral epicondylalgia: a clinical commentary". The Journal of Manual & Manipulative Therapy. 15 (1): 50–56. doi:10.1179/106698107791090132. PMC 2565595. PMID 19066643.
- ^ Herd CR, Meserve BB (2008-10-01). "A systematic review of the effectiveness of manipulative therapy in treating lateral epicondylalgia". The Journal of Manual & Manipulative Therapy. 16 (4): 225–237. doi:10.1179/106698108790818288. PMC 2716156. PMID 19771195.
- ^ Bjordal JM, Lopes-Martins RA, Joensen J, Couppe C, Ljunggren AE, Stergioulas A, Johnson MI (May 2008). "A systematic review with procedural assessments and meta-analysis of low level laser therapy in lateral elbow tendinopathy (tennis elbow)". BMC Musculoskeletal Disorders. 9 (1): 75. doi:10.1186/1471-2474-9-75. PMC 2442599. PMID 18510742.
- ^ Hoogvliet P, Randsdorp MS, Dingemanse R, Koes BW, Huisstede BM (November 2013). "Does effectiveness of exercise therapy and mobilisation techniques offer guidance for the treatment of lateral and medial epicondylitis? A systematic review". British Journal of Sports Medicine. 47 (17): 1112–1119. doi:10.1136/bjsports-2012-091990. PMID 23709519. S2CID 1679092.
- ^ Jayanthi N. "Epicondylitis (tennis and golf elbow)". UpToDate. UpToDate, Inc. Retrieved 17 August 2015.
- ^ a b Pattanittum P, Turner T, Green S, Buchbinder R (May 2013). "Non-steroidal anti-inflammatory drugs (NSAIDs) for treating lateral elbow pain in adults". The Cochrane Database of Systematic Reviews. 5 (5): CD003686. doi:10.1002/14651858.CD003686.pub2. PMC 7173751. PMID 23728646.
- ^ Krogh TP, Bartels EM, Ellingsen T, Stengaard-Pedersen K, Buchbinder R, Fredberg U, et al. (June 2013). "Comparative effectiveness of injection therapies in lateral epicondylitis: a systematic review and network meta-analysis of randomized controlled trials". The American Journal of Sports Medicine. 41 (6): 1435–1446. doi:10.1177/0363546512458237. PMID 22972856. S2CID 25355427.
- ^ a b Coombes BK, Bisset L, Vicenzino B (November 2010). "Efficacy and safety of corticosteroid injections and other injections for management of tendinopathy: a systematic review of randomised controlled trials". Lancet. 376 (9754): 1751–1767. doi:10.1016/S0140-6736(10)61160-9. hdl:10072/35812. PMID 20970844. S2CID 45054853.
- ^ Haines T, Stringer B (April 2007). "Corticosteroid injections or physiotherapy were not more effective than wait and see for tennis elbow at 1 year". Evidence-Based Medicine. 12 (2): 39. doi:10.1136/ebm.12.2.39. PMID 17400631. S2CID 43254510.
- ^ Coombes BK, Bisset L, Brooks P, Khan A, Vicenzino B (February 2013). "Effect of corticosteroid injection, physiotherapy, or both on clinical outcomes in patients with unilateral lateral epicondylalgia: a randomized controlled trial". JAMA. 309 (5): 461–469. doi:10.1001/jama.2013.129. hdl:10072/55521. PMID 23385272.
- ^ Buchbinder R, Green SE, Youd JM, Assendelft WJ, Barnsley L, Smidt N (October 2005). "Shock wave therapy for lateral elbow pain". The Cochrane Database of Systematic Reviews. 2009 (4): CD003524. doi:10.1002/14651858.cd003524.pub2. PMC 8717012. PMID 16235324.
- ^ Kalichman L, Bannuru RR, Severin M, Harvey W (June 2011). "Injection of botulinum toxin for treatment of chronic lateral epicondylitis: systematic review and meta-analysis". Seminars in Arthritis and Rheumatism. 40 (6): 532–538. doi:10.1016/j.semarthrit.2010.07.002. PMID 20822798. S2CID 22022658.
- ^ Monto R (September 2014). "Tennis elbow repair with or without suture anchors: a randomized clinical trial". Techniques in Shoulder and Elbow Surgery. 15 (3): 92–97. doi:10.1097/BTE.0000000000000027. S2CID 58020081.
- ^ a b Lo MY, Safran MR (October 2007). "Surgical treatment of lateral epicondylitis: a systematic review". Clinical Orthopaedics and Related Research. 463: 98–106. doi:10.1097/BLO.0b013e3181483dc4. PMID 17632419. S2CID 6954029.
- ^ Solheim E, Hegna J, Øyen J (May 2013). "Arthroscopic versus open tennis elbow release: 3- to 6-year results of a case-control series of 305 elbows". Arthroscopy. 29 (5): 854–859. doi:10.1016/j.arthro.2012.12.012. PMID 23388420.
- ^ Faro F, Wolf JM (October 2007). "Lateral epicondylitis: review and current concepts". The Journal of Hand Surgery. 32 (8): 1271–1279. doi:10.1016/j.jhsa.2007.07.019. PMID 17923315.
- ^ a b Bateman M, Littlewood C, Rawson B, Tambe AA (February 2019). "Surgery for tennis elbow: a systematic review". Shoulder & Elbow. 11 (1): 35–44. doi:10.1177/1758573217745041. PMC 6348580. PMID 30719096.
- ^ Buchbinder R, Johnston RV, Barnsley L, Assendelft WJ, Bell SN, Smidt N (March 2011). "Surgery for lateral elbow pain". The Cochrane Database of Systematic Reviews. 2011 (3): CD003525. doi:10.1002/14651858.cd003525.pub2. PMC 7154580. PMID 21412883.
- ^ Kroslak M, Murrell GA (April 2018). "Surgical Treatment of Lateral Epicondylitis: A Prospective, Randomized, Double-Blinded, Placebo-Controlled Clinical Trial". The American Journal of Sports Medicine. 46 (5): 1106–1113. doi:10.1177/0363546517753385. PMID 29498885. S2CID 4487650.
- ^ Drake ML, Ring DC (June 2016). "Enthesopathy of the Extensor Carpi Radialis Brevis Origin: Effective Communication Strategies". The Journal of the American Academy of Orthopaedic Surgeons. 24 (6): 365–369. doi:10.5435/JAAOS-D-15-00233. PMID 27077478. S2CID 19446305.
- ^ a b c d Shiri R, Viikari-Juntura E (February 2011). "Lateral and medial epicondylitis: role of occupational factors". Best Practice & Research. Clinical Rheumatology. 25 (1): 43–57. doi:10.1016/j.berh.2011.01.013. PMID 21663849.
- ^ a b "Tennis Elbow-Cap". The Lancet. 128 (3301): 1083. 1886. doi:10.1016/s0140-6736(00)49587-5.
- ^ Runge F (1873). "Zur Genese und Behandlung des Schreibekrampfes". Berliner Klin Wochenschr. 10: 245–248.
- ^ Renstrom PA (5 November 2013). "Elbow Injuries in Tennis". In Reilly T, Hughes M, Lees A (eds.). Science and Racket Sports. E & FN Spon. ISBN 978-0-419-18500-0.
- ^ Flatt AE (October 2008). "Tennis elbow". Proceedings. 21 (4): 400–402. doi:10.1080/08998280.2008.11928437. PMC 2566914. PMID 18982084.
- ^ Major HP (1883). "Lawn-tennis elbow". BMJ. 2 (1185): 556–558. doi:10.1136/bmj.2.1185.556. PMC 2372911.
- ^ Kaminsky SB, Baker CL (December 2003). "Lateral epicondylitis of the elbow". Techniques in Hand & Upper Extremity Surgery. 7 (4): 179–189. doi:10.1097/00130911-200312000-00009. PMID 16518219. S2CID 128648.
External links
[edit]- Wilson JJ, Best TM (September 2005). "Common overuse tendon problems: A review and recommendations for treatment". American Family Physician. 72 (5): 811–818. PMID 16156339. Archived from the original on 2007-09-29. Retrieved 2006-03-11.
