Obsessive–compulsive disorder
| Obsessive–compulsive disorder | |
|---|---|
 | |
| Frequent and excessive hand washing occurs in some people with OCD. | |
| Specialty | Psychiatry |
| Symptoms | Feel the need to check things repeatedly, perform certain routines repeatedly, have certain thoughts repeatedly[1] |
| Complications | Tics, anxiety disorder, suicide[2][3] |
| Usual onset | Before 35 years[1][2] |
| Risk factors | Genetics, biology, temperament, childhood trauma[1] |
| Diagnostic method | Clinically based on symptoms; Y-BOCS is the gold standard tool to assess severity[2] |
| Differential diagnosis | Anxiety disorder, major depressive disorder, eating disorders, tic disorders, obsessive–compulsive personality disorder[2] |
| Treatment | Counseling, selective serotonin reuptake inhibitors, clomipramine[4][5] |
| Frequency | 2.3%[6] |
Obsessive–compulsive disorder (OCD) is a mental and behavioral disorder in which an individual has intrusive thoughts (an obsession) and feels the need to perform certain routines (compulsions) repeatedly to relieve the distress caused by the obsession, to the extent where it impairs general function.[1][2][7]
Obsessions are persistent unwanted thoughts, mental images, or urges that generate feelings of anxiety, disgust, or discomfort.[8] Some common obsessions include fear of contamination, obsession with symmetry, the fear of acting blasphemously, the sufferer's sexual orientation, and the fear of possibly harming others or themselves.[1][9] Compulsions are repeated actions or routines that occur in response to obsessions to achieve a relief from anxiety. Common compulsions include excessive hand washing, cleaning, counting, ordering, repeating, avoiding triggers, hoarding, neutralizing, seeking assurance, praying, and checking things.[1][9][10] People with OCD may only perform mental compulsions such as needing to know or remember things. While this is sometimes referred to as primarily obsessional obsessive–compulsive disorder (Pure O), it is also considered a misnomer due to associated mental compulsions and reassurance seeking behaviors that are consistent with OCD.[11]
Compulsions occur often and typically take up at least one hour per day, impairing one's quality of life.[1][9] Compulsions cause relief in the moment, but cause obsessions to grow over time due to the repeated reward-seeking behavior of completing the ritual for relief. Many adults with OCD are aware that their compulsions do not make sense, but they still perform them to relieve the distress caused by obsessions.[1][8][9][12] For this reason, thoughts and behaviors in OCD are usually considered egodystonic. In contrast, thoughts and behaviors in obsessive-compulsive personality disorder (OCPD) are usually considered egosyntonic, helping differentiate between the two.[13]
Although the exact cause of OCD is unknown, several regions of the brain have been implicated in its neuroanatomical model including the anterior cingulate cortex, orbitofrontal cortex, amygdala, and BNST.[14][1] The presence of a genetic component is evidenced by the increased likelihood for both identical twins to be affected than both fraternal twins.[15] Risk factors include a history of child abuse or other stress-inducing events such as during the postpartum period or after streptococcal infections.[1][16] Diagnosis is based on clinical presentation and requires ruling out other drug-related or medical causes; rating scales such as the Yale–Brown Obsessive–Compulsive Scale (Y-BOCS) assess severity.[2][17] Other disorders with similar symptoms include generalized anxiety disorder, major depressive disorder, eating disorders, tic disorders, body-focused repetitive behavior, and obsessive–compulsive personality disorder.[2] Personality disorders are a common comorbidity, with schizotypal and OCPD having poor treatment response.[13] The condition is also associated with a general increase in suicidality.[3][18][19] The phrase obsessive–compulsive is sometimes used in an informal manner unrelated to OCD to describe someone as excessively meticulous, perfectionistic, absorbed, or otherwise fixated.[20] However, the actual disorder can vary in presentation, and individuals with OCD may not be concerned with cleanliness or symmetry.
OCD is chronic and long-lasting with periods of severe symptoms followed by periods of improvement.[21][22] Treatment can improve ability to function and quality of life, and is usually reflected by improved Y-BOCS scores.[23] Treatment for OCD may involve psychotherapy, pharmacotherapy such as antidepressants, or surgical procedures such as deep brain stimulation or, in extreme cases, psychosurgery.[4][5][24][25] Psychotherapies derived from cognitive behavioral therapy (CBT) models, such as exposure and response prevention, acceptance and commitment therapy, and inference based-therapy, are more effective than non-CBT interventions.[26] SSRIs are more effective when used in excess of the recommended depression dosage; however, higher doses can increase side effect intensity.[27] Commonly used SSRIs include sertraline, fluoxetine, fluvoxamine, paroxetine, citalopram, and escitalopram.[24] Some patients fail to improve after taking the maximum tolerated dose of multiple SSRIs for at least two months; these cases qualify as treatment-resistant and can require second-line treatment such as clomipramine or atypical antipsychotic augmentation.[4][5][27][28] While SSRIs continue to be first-line, recent data for treatment-resistant OCD supports adjunctive use of neuroleptic medications, deep-brain stimulation, and neurosurgical ablation.[29] There is growing evidence to support the use of deep brain stimulation and repetitive transcranial magnetic stimulation for treatment-resistant obsessive-compulsive disorder.[30][31]
Obsessive–compulsive disorder affects about 2.3% of people at some point in their lives, while rates during any given year are about 1.2%.[2][6] More than three million Americans suffer from OCD.[32] According to Mercy, approximately 1 in 40 U.S. adults and 1 in 100 U.S. children have OCD.[33] Although possible at times with triggers such as pregnancy, onset rarely occurs after age 35, and about 50% of patients experience detrimental effects to daily life before age 20.[1][16][2][34] While OCD occurs worldwide,[1][2] a recent meta-analysis showed that women are 1.6 times more likely to experience OCD.[35] Based on data from 34 studies, the worldwide prevalence rate is 1.5% in women and 1% in men.[35]
Signs and symptoms
OCD can present with a wide variety of symptoms. Certain groups of symptoms usually occur together as dimensions or clusters, which may reflect an underlying process. The standard assessment tool for OCD, the Yale–Brown Obsessive Compulsive Scale (Y-BOCS), has 13 predefined categories of symptoms. These symptoms fit into three to five groupings.[36] A meta-analytic review of symptom structures found a four-factor grouping structure to be most reliable: symmetry factor, forbidden thoughts factor, cleaning factor, and hoarding factor. The symmetry factor correlates highly with obsessions related to ordering, counting, and symmetry, as well as repeating compulsions. The forbidden thoughts factor correlates highly with intrusive thoughts of a violent, religious, or sexual nature. The cleaning factor correlates highly with obsessions about contamination and compulsions related to cleaning. The hoarding factor only involves hoarding-related obsessions and compulsions, and was identified as being distinct from other symptom groupings.[37]
When looking into the onset of OCD, one study suggests that there are differences in the age of onset between males and females, with the average age of onset of OCD being 9.6 for male children and 11.0 for female children.[38] Children with OCD often have other mental disorders, such as ADHD, depression, anxiety, and disruptive behavior disorder. Continually, children are more likely to struggle in school and experience difficulties in social situations (Lack 2012). When looking at both adults and children a study found the average ages of onset to be 21 and 24 for males and females respectively.[39] While some studies have shown that OCD with earlier onset is associated with greater severity, other studies have not been able to validate this finding.[40] Looking at women specifically, a different study suggested that 62% of participants found that their symptoms worsened at a premenstrual age. Across the board, all demographics and studies showed a mean age of onset of less than 25.[41]
Some OCD subtypes have been associated with improvement in performance on certain tasks, such as pattern recognition (washing subtype) and spatial working memory (obsessive thought subtype). Subgroups have also been distinguished by neuroimaging findings and treatment response, though neuroimaging studies have not been comprehensive enough to draw conclusions. Subtype-dependent treatment response has been studied, and the hoarding subtype has consistently been least responsive to treatment.[42]
While OCD is considered a homogeneous disorder from a neuropsychological perspective, many of the symptoms may be the result of comorbid disorders. For example, adults with OCD have exhibited more symptoms of attention–deficit/hyperactivity disorder (ADHD) and autism spectrum disorder (ASD) than adults without OCD.[43]
In regards to the cause of onset, researchers asked participants in one study[41] what they felt was responsible for triggering the initial onset of their illness. 29% of patients answered that there was an environmental factor in their life that did so. Specifically, the majority of participants who answered with that noted their environmental factor to be related to an increased responsibility.
Obsessions

Obsessions are stress-inducing thoughts that recur and persist, despite efforts to ignore or confront them.[44] People with OCD frequently perform tasks, or compulsions, to seek relief from obsession-related anxiety. Within and among individuals, initial obsessions vary in clarity and vividness. A relatively vague obsession could involve a general sense of disarray or tension, accompanied by a belief that life cannot proceed as normal while the imbalance remains. A more intense obsession could be a preoccupation with the thought or image of a close family member or friend dying, or intrusive thoughts related to relationship rightness.[45][46] Other obsessions concern the possibility that someone or something other than oneself—such as God, the devil, or disease—will harm either the patient or the people or things the patient cares about. Others with OCD may experience the sensation of invisible protrusions emanating from their bodies, or feel that inanimate objects are ensouled.[47] Another common obsession is scrupulosity, the pathological guilt/anxiety about moral or religious issues. In scrupulosity, a person's obsessions focus on moral or religious fears, such as the fear of being an evil person or the fear of divine retribution for sin.[48][49] Mysophobia, a pathological fear of contamination and germs, is another common obsession theme.[50][51]
Some people with OCD experience sexual obsessions that may involve intrusive thoughts or images of "kissing, touching, fondling, oral sex, anal sex, intercourse, incest, and rape" with "strangers, acquaintances, parents, children, family members, friends, coworkers, animals, and religious figures", and can include heterosexual or homosexual contact with people of any age.[52] Similar to other intrusive thoughts or images, some disquieting sexual thoughts are normal at times, but people with OCD may attach extraordinary significance to such thoughts. For example, obsessive fears about sexual orientation can appear to the affected individual, and even to those around them, as a crisis of sexual identity.[53][54] Furthermore, the doubt that accompanies OCD leads to uncertainty regarding whether one might act on the troubling thoughts, resulting in self-criticism or self-loathing.[52]
Most people with OCD understand that their thoughts do not correspond with reality; however, they feel that they must act as though these ideas are correct or realistic. For example, someone who engages in compulsive hoarding might be inclined to treat inorganic matter as if it had the sentience or rights of living organisms, despite accepting that such behavior is irrational on an intellectual level. There is debate as to whether hoarding should be considered an independent syndrome from OCD.[55]
Compulsions

Some people with OCD perform compulsive rituals because they inexplicably feel that they must do so, while others act compulsively to mitigate the anxiety that stems from obsessive thoughts. The affected individual might feel that these actions will either prevent a dreaded event from occurring, or push the event from their thoughts. In any case, their reasoning is so idiosyncratic or distorted that it results in significant distress, either personally, or for those around the affected individual. Excessive skin picking, hair pulling, nail biting, and other body-focused repetitive behavior disorders are all on the obsessive–compulsive spectrum.[2] Some individuals with OCD are aware that their behaviors are not rational, but they feel compelled to follow through with them to fend off feelings of panic or dread.[56] Furthermore, compulsions often stem from memory distrust, a symptom of OCD characterized by insecurity in one's skills in perception, attention, and memory, even in cases where there is no clear evidence of a deficit.[57]
Common compulsions may include hand washing, cleaning, checking things (such as locks on doors), repeating actions (such as repeatedly turning on and off switches), ordering items in a certain way, and requesting reassurance.[58][59] Although some individuals perform actions repeatedly, they do not necessarily perform these actions compulsively; for example, morning or nighttime routines and religious practices are not usually compulsions. Whether behaviors qualify as compulsions or mere habit depends on the context in which they are performed. For instance, arranging and ordering books for eight hours a day would be expected of someone who works in a library, but this routine would seem abnormal in other situations. In other words, habits tend to bring efficiency to one's life, while compulsions tend to disrupt it.[60] Furthermore, compulsions are different from tics (such as touching, tapping, rubbing, or blinking) and stereotyped movements (such as head banging, body rocking, or self-biting), which are usually not as complex and not precipitated by obsessions.[61] It can sometimes be difficult to tell the difference between compulsions and complex tics, and about 10–40% of people with OCD also have a lifetime tic disorder.[2][62]
People with OCD rely on compulsions as an escape from their obsessive thoughts; however, they are aware that relief is only temporary, and that intrusive thoughts will return. Some affected individuals use compulsions to avoid situations that may trigger obsessions. Compulsions may be actions directly related to the obsession, such as someone obsessed with contamination compulsively washing their hands, but they can be unrelated as well.[9] In addition to experiencing the anxiety and fear that typically accompanies OCD, affected individuals may spend hours performing compulsions every day. In such situations, it can become difficult for the person to fulfill their work, familial, or social roles. These behaviors can also cause adverse physical symptoms; for example, people who obsessively wash their hands with antibacterial soap and hot water can make their skin red and raw with dermatitis.[63]
Individuals with OCD often use rationalizations to explain their behavior; however, these rationalizations do not apply to the behavioral pattern, but to each individual occurrence. For example, someone compulsively checking the front door may argue that the time and stress associated with one check is less than the time and stress associated with being robbed, and checking is consequently the better option. This reasoning often occurs in a cyclical manner, and can continue for as long as the affected person needs it to in order to feel safe.[64]
In cognitive behavioral therapy (CBT), OCD patients are asked to overcome intrusive thoughts by not indulging in any compulsions. They are taught that rituals keep OCD strong, while not performing them causes OCD to become weaker.[65] This position is supported by the pattern of memory distrust; the more often compulsions are repeated, the more weakened memory trust becomes, and this cycle continues as memory distrust increases compulsion frequency.[66] For body-focused repetitive behaviors (BFRB) such as trichotillomania (hair pulling), skin picking, and onychophagia (nail biting), behavioral interventions such as habit reversal training and decoupling are recommended for the treatment of compulsive behaviors.[67][68]
OCD sometimes manifests without overt compulsions, which may be termed "primarily obsessional OCD." OCD without overt compulsions could, by one estimate, characterize as many as 50–60% of OCD cases.[69]
Insight and overvalued ideation
The Diagnostic and Statistical Manual of Mental Disorders (DSM-5), identifies a continuum for the level of insight in OCD, ranging from good insight (the least severe) to no insight (the most severe). Good or fair insight is characterized by the acknowledgment that obsessive–compulsive beliefs are not or may not be true, while poor insight, in the middle of the continuum, is characterized by the belief that obsessive–compulsive beliefs are probably true. The absence of insight altogether, in which the individual is completely convinced that their beliefs are true, is also identified as a delusional thought pattern, and occurs in about 4% of people with OCD.[70][71] When cases of OCD with no insight become severe, affected individuals have an unshakable belief in the reality of their delusions, which can make their cases difficult to differentiate from psychotic disorders.[72]
Some people with OCD exhibit what is known as overvalued ideas, ideas that are abnormal compared to affected individuals' respective cultures, and more treatment-resistant than most negative thoughts and obsessions.[73] After some discussion, it is possible to convince the individual that their fears are unfounded. It may be more difficult to practice exposure and response prevention therapy (ERP) on such people, as they may be unwilling to cooperate, at least initially.[74] Similar to how insight is identified on a continuum, obsessive-compulsive beliefs are characterized on a spectrum, ranging from obsessive doubt to delusional conviction. In the United States, overvalued ideation (OVI) is considered most akin to poor insight—especially when considering belief strength as one of an idea's key identifiers.[75] Furthermore, severe and frequent overvalued ideas are considered similar to idealized values, which are so rigidly held by, and so important to affected individuals, that they end up becoming a defining identity.[73] In adolescent OCD patients, OVI is considered a severe symptom.[76]
Historically, OVI has been thought to be linked to poorer treatment outcome in patients with OCD, but it is currently considered a poor indicator of prognosis.[76][77] The Overvalued Ideas Scale (OVIS) has been developed as a reliable quantitative method of measuring levels of OVI in patients with OCD, and research has suggested that overvalued ideas are more stable for those with more extreme OVIS scores.[78]
Cognitive performance
Though OCD was once believed to be associated with above-average intelligence, this does not appear to necessarily be the case.[79] A 2013 review reported that people with OCD may sometimes have mild but wide-ranging cognitive deficits, most significantly those affecting spatial memory and to a lesser extent with verbal memory, fluency, executive function, and processing speed, while auditory attention was not significantly affected.[80] People with OCD show impairment in formulating an organizational strategy for coding information, set-shifting, and motor and cognitive inhibition.[81]
Specific subtypes of symptom dimensions in OCD have been associated with specific cognitive deficits.[82] For example, the results of one meta-analysis comparing washing and checking symptoms reported that washers outperformed checkers on eight out of ten cognitive tests.[83] The symptom dimension of contamination and cleaning may be associated with higher scores on tests of inhibition and verbal memory.[84]
Video game addiction
Pediatric OCD
Approximately 1–2% of children are affected by OCD.[86] There is a lot of similarity between the clinical presentation of OCD in children and adults, and it is considered a highly familial disorder, with a phenotypic heritability of around 50%.[38][87] Obsessive–compulsive disorder symptoms tend to develop more frequently in children 10–14 years of age, with males displaying symptoms at an earlier age, and at a more severe level than females.[88] In children, symptoms can be grouped into at least four types, including sporadic and tic-related OCD.[36]
The Children's Yale–Brown Obsessive–Compulsive Scale (CY-BOCS) is the gold standard measure for assessment of pediatric OCD.[89] It follows the Y-BOCS format, but with a Symptom Checklist that is adapted for developmental appropriateness. Insight, avoidance, indecisiveness, responsibility, pervasive slowness, and doubting, are not included in a rating of overall severity. The CY-BOCS has demonstrated good convergent validity with clinician-rated OCD severity, and good to fair discriminant validity from measures of closely related anxiety, depression, and tic severity.[89] The CY-BOCS Total Severity score is an important monitoring tool as it is responsive to pharmacotherapy and psychotherapy.[90][91] Positive treatment response is characterized by 25% reduction in CY-BOCS total score, and diagnostic remission is associated with a 45%-50% reduction in Total Severity score (or a score <15).[89]
CBT is the first line treatment for mild to moderate cases of OCD in children, while medication plus CBT is recommended for moderate to severe cases.[92][93][94] Serotonin reuptake inhibitors (SRIs) are first-line medications for OCD in children with established AACAP guidelines for dosing.[95]
Associated conditions
People with OCD may be diagnosed with other conditions as well, such as obsessive–compulsive personality disorder, major depressive disorder, bipolar disorder, generalized anxiety disorder, anorexia nervosa, social anxiety disorder, bulimia nervosa, Tourette syndrome, transformation obsession, ASD, ADHD, dermatillomania, body dysmorphic disorder, and trichotillomania.[96] More than 50% of people with OCD experience suicidal tendencies, and 15% have attempted suicide.[17] Depression, anxiety, and prior suicide attempts increase the risk of future suicide attempts.[97]
It has been found that between 18 and 34% of females currently experiencing OCD scored positively on an inventory measuring disordered eating.[98] Another study found that 7% are likely to have an eating disorder,[98] while another found that fewer than 5% of males have OCD and an eating disorder.[99]
Individuals with OCD have also been found to be affected by delayed sleep phase disorder at a substantially higher rate than the general public.[100][101] Moreover, severe OCD symptoms are consistently associated with greater sleep disturbance. Reduced total sleep time and sleep efficiency have been observed in people with OCD, with delayed sleep onset and offset.[101]
Some research has demonstrated a link between drug addiction and OCD. For example, there is a higher risk of drug addiction among those with any anxiety disorder, likely as a way of coping with the heightened levels of anxiety. However, drug addiction among people with OCD may be a compulsive behavior. Depression is also extremely prevalent among people with OCD. One explanation for the high depression rate among OCD populations was posited by Mineka, Watson, and Clark (1998), who explained that people with OCD, or any other anxiety disorder, may feel "out of control".[102]
Someone exhibiting OCD signs does not necessarily have OCD. Behaviors that present as obsessive–compulsive can also be found in a number of other conditions, including obsessive–compulsive personality disorder (OCPD), autism spectrum disorder (ASD), or disorders in which perseveration is a possible feature (ADHD, PTSD, bodily disorders, or stereotyped behaviors).[103] Some cases of OCD present symptoms typically associated with Tourette syndrome, such as compulsions that may appear to resemble motor tics; this has been termed tic-related OCD or Tourettic OCD.[104][105]
OCD frequently occurs comorbidly with both bipolar disorder and major depressive disorder. Between 60 and 80% of those with OCD experience a major depressive episode in their lifetime. Comorbidity rates have been reported at between 19 and 90%, as a result of methodological differences. Between 9–35% of those with bipolar disorder also have OCD, compared to 1–2% in the general population. About 50% of those with OCD experience cyclothymic traits or hypomanic episodes. OCD is also associated with anxiety disorders. Lifetime comorbidity for OCD has been reported at 22% for specific phobia, 18% for social anxiety disorder, 12% for panic disorder, and 30% for generalized anxiety disorder. The comorbidity rate for OCD and ADHD has been reported to be as high as 51%.[106]
Causes
The cause of OCD is unknown.[1] Both environmental and genetic factors are believed to play a role. Risk factors include a history of adverse childhood experiences or other stress-inducing events.[2][107][108]
Drug-induced OCD
Some medications, toxin exposures, and drugs, such as methamphetamine or cocaine, can induce obsessive-compulsive disorder (OCD) in people without previous symptoms.[108] Some atypical antipsychotics (second-generation antipsychotics) such as olanzapine (Zyprexa) and clozapine (Clozaril) can induce OCD in people, particularly individuals with schizophrenia.
The diagnostic criteria include:
1) General OCD symptoms (obsessions, compulsions, skin picking, hair pulling, etc.) that developed soon after exposure to the substance or medication which can produce such symptoms.
2) The onset of symptoms cannot be explained by an obsessive-compulsive and related disorder that is not substance/medication-induced and should last for a substantial period of time (about 1 month)
3) This disturbance does not only occur during delirium.
4) Clinically induces distress or impairment in social, occupational, or other important areas of functioning. [109][110][111][112][113]
Genetics
There appear to be some genetic components of OCD causation, with identical twins more often affected than fraternal twins.[2] Furthermore, individuals with OCD are more likely to have first-degree family members exhibiting the same disorders than matched controls. In cases in which OCD develops during childhood, there is a much stronger familial link in the disorder than with cases in which OCD develops later in adulthood. In general, genetic factors account for 45–65% of the variability in OCD symptoms in children diagnosed with the disorder.[114] A 2007 study found evidence supporting the possibility of a heritable risk for OCD.[115]
Research has found there to be a genetic correlation between anorexia nervosa and OCD, suggesting a strong etiology.[116][117][118] First and second hand relatives of probands with OCD have a greater risk of developing anorexia nervosa as genetic relatedness increases.[116]
A mutation has been found in the human serotonin transporter gene hSERT in unrelated families with OCD.[119]
A systematic review found that while neither allele was associated with OCD overall, in Caucasians, the L allele was associated with OCD.[120] Another meta-analysis observed an increased risk in those with the homozygous S allele, but found the LS genotype to be inversely associated with OCD.[121]
A genome-wide association study found OCD to be linked with single-nucleotide polymorphisms (SNPs) near BTBD3, and two SNPs in DLGAP1 in a trio-based analysis, but no SNP reached significance when analyzed with case-control data.[122]
One meta-analysis found a small but significant association between a polymorphism in SLC1A1 and OCD.[123]
The relationship between OCD and Catechol-O-methyltransferase (COMT) has been inconsistent, with one meta-analysis reporting a significant association, albeit only in men, and another meta analysis reporting no association.[124][125]
It has been postulated by evolutionary psychologists that moderate versions of compulsive behavior may have had evolutionary advantages. Examples would be moderate constant checking of hygiene, the hearth, or the environment for enemies. Similarly, hoarding may have had evolutionary advantages. In this view, OCD may be the extreme statistical tail of such behaviors, possibly the result of a high number of predisposing genes.[126]
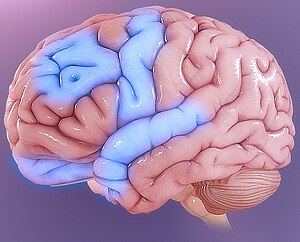
Brain structure and functioning
Imaging studies have shown differences in the frontal cortex and subcortical structures of the brain in patients with OCD. There appears to be a connection between the OCD symptoms and abnormalities in certain areas of the brain, but such a connection is not clear.[21] Some people with OCD have areas of unusually high activity in their brain, or low levels of the chemical serotonin,[127] which is a neurotransmitter that some nerve cells use to communicate with each other,[128] and is thought to be involved in regulating many functions, influencing emotions, mood, memory, and sleep.[129]
Autoimmune
A controversial hypothesis is that some cases of rapid onset of OCD in children and adolescents may be caused by a syndrome connected to Group A streptococcal infections (GABHS), known as pediatric autoimmune neuropsychiatric disorders associated with streptococcal infections (PANDAS).[130][131][132] OCD and tic disorders are hypothesized to arise in a subset of children as a result of a post-streptococcal autoimmune process.[133][134][135] The PANDAS hypothesis is unconfirmed and unsupported by data, and two new categories have been proposed: PANS (pediatric acute-onset neuropsychiatric syndrome) and CANS (childhood acute neuropsychiatric syndrome).[134][135] The CANS and PANS hypotheses include different possible mechanisms underlying acute-onset neuropsychiatric conditions, but do not exclude GABHS infections as a cause in a subset of individuals.[134][135] PANDAS, PANS, and CANS are the focus of clinical and laboratory research, but remain unproven.[133][134][135] Whether PANDAS is a distinct entity differing from other cases of tic disorders or OCD is debated.[136][137][138][139]
A review of studies examining anti-basal ganglia antibodies in OCD found an increased risk of having anti-basal ganglia antibodies in those with OCD versus the general population.[140]
Environment
OCD may be more common in people who have been bullied, abused, or neglected, and it sometimes starts after a significant life event, such as childbirth or bereavement.[127] It has been reported in some studies that there is a connection between childhood trauma and obsessive-compulsive symptoms. More research is needed to understand this relationship better.[21]
Mechanisms
Neuroimaging
Functional neuroimaging during symptom provocation has observed abnormal activity in the orbitofrontal cortex (OFC), left dorsolateral prefrontal cortex (dlPFC), right premotor cortex, left superior temporal gyrus, globus pallidus externus, hippocampus, and right uncus. Weaker foci of abnormal activity were found in the left caudate, posterior cingulate cortex, and superior parietal lobule.[141] However, an older meta-analysis of functional neuroimaging in OCD reported that the only consistent functional neuroimaging finding was increased activity in the orbital gyrus and head of the caudate nucleus, while anterior cingulate cortex (ACC) activation abnormalities were too inconsistent.[142]
A meta-analysis comparing affective and nonaffective tasks observed differences with controls in regions implicated in salience, habit, goal-directed behavior, self-referential thinking, and cognitive control. For nonaffective tasks, hyperactivity was observed in the insula, ACC, and head of the caudate/putamen, while hypoactivity was observed in the medial prefrontal cortex (mPFC) and posterior caudate. Affective tasks were observed to relate to increased activation in the precuneus and posterior cingulate cortex, while decreased activation was found in the pallidum, ventral anterior thalamus, and posterior caudate.[143] The involvement of the cortico-striato-thalamo-cortical loop in OCD, as well as the high rates of comorbidity between OCD and ADHD, have led some to draw a link in their mechanism. Observed similarities include dysfunction of the anterior cingulate cortex and prefrontal cortex, as well as shared deficits in executive functions.[144] The involvement of the orbitofrontal cortex and dorsolateral prefrontal cortex in OCD is shared with bipolar disorder, and may explain the high degree of comorbidity.[145] Decreased volumes of the dorsolateral prefrontal cortex related to executive function has also been observed in OCD.[146]
People with OCD evince increased grey matter volumes in bilateral lenticular nuclei, extending to the caudate nuclei, with decreased grey matter volumes in bilateral dorsal medial frontal/anterior cingulate gyri.[147][145] These findings contrast with those in people with other anxiety disorders, who evince decreased (rather than increased) grey matter volumes in bilateral lenticular/caudate nuclei, as well as decreased grey matter volumes in bilateral dorsal medial frontal/anterior cingulate gyri.[145] Increased white matter volume and decreased fractional anisotropy in anterior midline tracts has been observed in OCD, possibly indicating increased fiber crossings.[148]
Cognitive models
Generally, two categories of models for OCD have been postulated. The first category involves deficits in executive dysfunction and is based on the observed structural and functional abnormalities in the dlPFC, striatum and thalamus. The second category involves dysfunctional modulatory control and primarily relies on observed functional and structural differences in the ACC, mPFC, and OFC.[149][150]
One proposed model suggests that dysfunction in the OFC leads to improper valuation of behaviors and decreased behavioral control, while the observed alterations in amygdala activations leads to exaggerated fears and representations of negative stimuli.[151]
Due to the heterogeneity of OCD symptoms, studies differentiating various symptoms have been performed. Symptom-specific neuroimaging abnormalities include the hyperactivity of caudate and ACC in checking rituals, while finding increased activity of cortical and cerebellar regions in contamination-related symptoms. Neuroimaging differentiating content of intrusive thoughts has found differences between aggressive as opposed to taboo thoughts, finding increased connectivity of the amygdala, ventral striatum, and ventromedial prefrontal cortex in aggressive symptoms, while observing increased connectivity between the ventral striatum and insula in sexual or religious intrusive thoughts.[152]
Another model proposes that affective dysregulation links excessive reliance on habit-based action selection[153] with compulsions. This is supported by the observation that those with OCD demonstrate decreased activation of the ventral striatum when anticipating monetary reward, as well as increased functional connectivity between the VS and the OFC. Furthermore, those with OCD demonstrate reduced performance in Pavlovian fear-extinction tasks, hyperresponsiveness in the amygdala to fearful stimuli, and hyporesponsiveness in the amygdala when exposed to positively valanced stimuli. Stimulation of the nucleus accumbens has also been observed to effectively alleviate both obsessions and compulsions, supporting the role of affective dysregulation in generating both.[151]
Neurobiological
From the observation of the efficacy of antidepressants in OCD, a serotonin hypothesis of OCD has been formulated. Studies of peripheral markers of serotonin, as well as challenges with proserotonergic compounds have yielded inconsistent results, including evidence pointing towards basal hyperactivity of serotonergic systems.[154] Serotonin receptor and transporter binding studies have yielded conflicting results, including higher and lower serotonin receptor 5-HT2A and serotonin transporter binding potentials that were normalized by treatment with SSRIs. Despite inconsistencies in the types of abnormalities found, evidence points towards dysfunction of serotonergic systems in OCD.[155] Orbitofrontal cortex overactivity is attenuated in people who have successfully responded to SSRI medication, a result believed to be caused by increased stimulation of serotonin receptors 5-HT2A and 5-HT2C.[156]
A complex relationship between dopamine and OCD has been observed. Although antipsychotics, which act by antagonizing dopamine receptors, may improve some cases of OCD, they frequently exacerbate others. Antipsychotics, in the low doses used to treat OCD, may actually increase the release of dopamine in the prefrontal cortex, through inhibiting autoreceptors. Further complicating things is the efficacy of amphetamines, decreased dopamine transporter activity observed in OCD,[157] and low levels of D2 binding in the striatum.[158] Furthermore, increased dopamine release in the nucleus accumbens after deep brain stimulation correlates with improvement in symptoms, pointing to reduced dopamine release in the striatum playing a role in generating symptoms.[159]
Abnormalities in glutamatergic neurotransmission have been implicated in OCD. Findings such as increased cerebrospinal glutamate, less consistent abnormalities observed in neuroimaging studies, and the efficacy of some glutamatergic drugs (such as the glutamate-inhibiting riluzole) have implicated glutamate in OCD.[158] OCD has been associated with reduced N-Acetylaspartic acid in the mPFC, which is thought to reflect neuron density or functionality, although the exact interpretation has not been established.[160]
Diagnosis
Formal diagnosis may be performed by a psychologist, psychiatrist, clinical social worker, or other licensed mental health professional. OCD, like other mental and behavioral health disorders, cannot be diagnosed by a medical exam,[7] nor are there any medical exams that can predict if one will fall victim to such illnesses. To be diagnosed with OCD, a person must have obsessions, compulsions, or both, according to the Diagnostic and Statistical Manual of Mental Disorders (DSM). The DSM notes that there are multiple characteristics that can turn obsessions and compulsions from normalized behavior to "clinically significant". There has to be recurring and strong thoughts or impulsive that intrude on the day-to-day lives of the patients and cause noticeable levels of anxiousness.[2]
These thoughts, impulses, or images are of a degree or type that lies outside the normal range of worries about conventional problems.[161] A person may attempt to ignore or suppress such obsessions, neutralize them with another thought or action, or try to rationalize their anxiety away. People with OCD tend to recognize their obsessions as irrational.
Compulsions become clinically significant when a person feels driven to perform them in response to an obsession, or according to rules that must be applied rigidly, and when the person consequently feels or causes significant distress. Therefore, while many people who do not have OCD may perform actions often associated with OCD (such as ordering items in a pantry by height), the distinction with clinically significant OCD lies in the fact that the person with OCD must perform these actions to avoid significant psychological distress. These behaviors or mental acts are aimed at preventing or reducing distress or preventing some dreaded event or situation; however, these activities are not logically or practically connected to the issue, or, they are excessive.
Moreover, the obsessions or compulsions must be time-consuming, often taking up more than one hour per day, or cause impairment in social, occupational, or scholastic functioning.[161] It is helpful to quantify the severity of symptoms and impairment before and during treatment for OCD. In addition to the person's estimate of the time spent each day harboring obsessive-compulsive thoughts or behaviors, concrete tools can be used to gauge the person's condition. This may be done with rating scales, such as the Yale–Brown Obsessive Compulsive Scale (Y-BOCS; expert rating)[162] or the obsessive-compulsive inventory (OCI-R; self-rating).[163] With measurements such as these, psychiatric consultation can be more appropriately determined, as it has been standardized.[17]
In regards to diagnosing, the health professional also looks to make sure that the signs of obsessions and compulsions are not the results of any drugs, prescription or recreational, that the patient may be taking.[164]
There are several types of obsessive thoughts that are found commonly in those with OCD. Some of these include fear of germs, hurting loved ones, embarrassment, neatness, societally unacceptable sexual thoughts etc.[164] Within OCD, these specific categories are often diagnosed into their own type of OCD.[2]
OCD is sometimes placed in a group of disorders called the obsessive–compulsive spectrum.[165]
Another criterion in the DSM is that a person's mental illness does not fit one of the other categories of a mental disorder better. That is to say, if the obsessions and compulsions of a patient could be better described by trichotillomania, it would not be diagnosed as OCD.[2] That being said, OCD does often go hand in hand with other mental disorders. For this reason, one may be diagnosed with multiple mental disorders at once.[166]
A different aspect of the diagnoses is the degree of insight had by the individual in regards to the truth of the obsessions. There are three levels, good/fair, poor and absent/delusional. Good/fair indicated that the patient is aware that the obsessions they have are not true or probably not true.[2] Poor indicates that the patient believes their obsessional beliefs are probably true.[2] Absent/delusional indicates that they fully believe their obsessional thoughts to be true.[2] Approximately 4% or fewer individuals with OCD will be diagnosed as absent/delusional.[2] Additionally, as many as 30% of those with OCD also have a lifetime tic disorder, meaning they have been diagnosed with a tic disorder at some point in their life.[2]
There are several different types of tics that have been observed in individuals with OCD. These include but are not limited to, "grunting", "jerking" or "shrugging" body parts, sniffling, and excessive blinking.[164]
There has been a significant amount of progress over the last few decades, and as of 2022 there is statically significant improvement in the diagnostic process for individuals with OCD. One study found that of two groups of individuals, one with participants under the age of 27.25 and one with participants over that age, those in the younger group experienced a significantly faster time between the onset of OCD tendencies and their formal diagnoses.[167]
Differential diagnosis
OCD is often confused with the separate condition obsessive–compulsive personality disorder (OCPD). OCD is egodystonic, meaning that the disorder is incompatible with the individual's self-concept.[168][169] As egodystonic disorders go against a person's self-concept, they tend to cause much distress. OCPD, on the other hand, is egosyntonic, marked by the person's acceptance that the characteristics and behaviors displayed as a result are compatible with their self-image, or are otherwise appropriate, correct, or reasonable.
As a result, people with OCD are often aware that their behavior is not rational, and are unhappy about their obsessions, but nevertheless feel compelled by them.[170] By contrast, people with OCPD are not aware of anything abnormal; they will readily explain why their actions are rational. It is usually impossible to convince them otherwise, and they tend to derive pleasure from their obsessions or compulsions.[170]
Management
Cognitive behavioral therapy (CBT) and psychotropic medications are the first-line treatments for OCD.[1][171]
Therapy

One specific CBT technique used is called exposure and response prevention (ERP), which involves teaching the person to deliberately come into contact with situations that trigger obsessive thoughts and fears (exposure), without carrying out the usual compulsive acts associated with the obsession (response prevention). This technique causes patients to gradually learn to tolerate the discomfort and anxiety associated with not performing their compulsions. For many patients, ERP is the add-on treatment of choice when selective serotonin reuptake inhibitors (SSRIs) or serotonin-norepinephrine reuptake inhibitors (SNRIs) medication does not effectively treat OCD symptoms, or vice versa, for individuals who begin treatment with psychotherapy.[21] This technique is considered superior to others due to the lack of medication used. However, up to 25% of patients will discontinue treatment due to the severity of their tics. CBT normally lasts anywhere from 12-16 sessions, with homework assigned to the patient in between meetings with a therapist. (Lack 2012). Modalities differ in ERP treatment but both virtual reality based as well as unguided computer assisted treatment programs have shown effective results in treatment programs.[172][173]
For example, a patient might be asked to touch something very mildly contaminated (exposure), and wash their hands only once afterward (response prevention). Another example might entail asking the patient to leave the house and check the lock only once (exposure), without going back to check again (response prevention). After succeeding at one stage of treatment, the patient's level of discomfort in the exposure phase can be increased. When this therapy is successful, the patient will quickly habituate to an anxiety-producing situation, discovering a considerable drop in anxiety level.[174]
ERP has a strong evidence base, and is considered the most effective treatment for OCD.[174] However, this claim was doubted by some researchers in 2000, who criticized the quality of many studies.[175] While ERP can lead a majority of clients to improvements, many do not reach remission or become asymptomatic;[176] some therapists are also hesitant to use this approach.[177]
The recent development of remotely technology-delivered CBT is increasing access to therapy options for those living with OCD and remote versions appear to equally as effective as in-person therapy options. The development of smartphone interventions for OCD that utilize CBT techniques are another alternative that is expanding access to therapy while allowing therapies to be personalized for each patient.[178]
Acceptance and commitment therapy (ACT), a newer therapy also used to treat anxiety and depression, has also been found to be effective in treatment of OCD.[179][180] ACT uses acceptance and mindfulness strategies to teach patients not to overreact to or avoid unpleasant thoughts and feelings but rather "move toward valued behavior."[181][182]
Inference-based therapy (IBT) is a form of cognitive therapy specifically developed for treating OCD.[183] The therapy posits that individuals with OCD put a greater emphasis on an imagined possibility than on what can be perceived with the senses, and confuse the imagined possibility with reality, in a process called inferential confusion.[184] According to inference-based therapy, obsessional thinking occurs when the person replaces reality and real probabilities with imagined possibilities.[185] The goal of inference-based therapy is to reorient clients towards trusting the senses and relating to reality in a normal, non-effortful way. Differences between normal and obsessional doubts are presented, and clients are encouraged to use their senses and reasoning as they do in non-obsessive-compulsive disorder situations.[186][183] Research on Inference-Based Cognitive-Behavior Therapy (I-CBT) suggests it can lead to improvements for those with OCD.[187]
A 2007 Cochrane review found that psychological interventions derived from CBT models, such as ERP, ACT, and IBT, were more effective than non-CBT interventions.[26] Other forms of psychotherapy, such as psychodynamics and psychoanalysis, may help in managing some aspects of the disorder. However, in 2007, the American Psychiatric Association (APA) noted a lack of controlled studies showing their efficacy, "in dealing with the core symptoms of OCD."[188] For body-focused repetitive behaviors (BFRB), behavioral interventions such as habit-reversal training and decoupling are recommended.[67][68]
Psychotherapy in combination with psychiatric medication may be more effective than either option alone for individuals with severe OCD.[189][190][191] ERP coupled with weight restoration and serotonin reuptake inhibitors has proven the most effective when treating OCD and an eating disorder simultaneously.[192]
Medication

The medications most frequently used to treat OCD are antidepressants, including selective serotonin reuptake inhibitors (SSRIs) and serotonin-norepinephrine reuptake inhibitors (SNRIs).[4] Sertraline and fluoxetine are effective in treating OCD for children and adolescents.[193][194][195]
SSRIs help people with OCD by inhibiting the reabsorption of serotonin by the nerve cells after they carry messages from neurons to synapse; thus, more serotonin is available to pass further messages between nearby nerve cells.[129][clarify]
SSRIs are a second-line treatment of adult OCD with mild functional impairment, and as first-line treatment for those with moderate or severe impairment. In children, SSRIs can be considered as a second-line therapy in those with moderate to severe impairment, with close monitoring for psychiatric adverse effects.[171] Patients treated with SSRIs are about twice as likely to respond to treatment as are those treated with placebo, so this treatment is qualified as efficacious.[196][197] Efficacy has been demonstrated both in short-term (6–24 weeks) treatment trials, and in discontinuation trials with durations of 28–52 weeks.[198][199][200]
Clomipramine, a medication belonging to the class of tricyclic antidepressants, appears to work as well as SSRIs, but has a higher rate of side effects.[4]
In 2006, the National Institute for Health and Care Excellence (NICE) guidelines recommended augmentative second-generation (atypical) antipsychotics for treatment-resistant OCD.[5] Atypical antipsychotics are not useful when used alone, and no evidence supports the use of first-generation antipsychotics.[28][201] For OCD treatment specifically, there is tentative evidence for risperidone, and insufficient evidence for olanzapine. Quetiapine is no better than placebo with regard to primary outcomes, but small effects were found in terms of Y-BOCS score. The efficacy of quetiapine and olanzapine are limited by an insufficient number of studies.[202] A 2014 review article found two studies that indicated that aripiprazole was "effective in the short-term", and found that "[t]here was a small effect-size for risperidone or anti-psychotics in general in the short-term"; however, the study authors found "no evidence for the effectiveness of quetiapine or olanzapine in comparison to placebo."[5] While quetiapine may be useful when used in addition to an SSRI/SNRI in treatment-resistant OCD, these drugs are often poorly tolerated, and have metabolic side effects that limit their use. A guideline by the American Psychological Association suggested that dextroamphetamine may be considered by itself after more well-supported treatments have been attempted.[203]
Procedures
Electroconvulsive therapy (ECT) has been found to have effectiveness in some severe and refractory cases.[204] Transcranial magnetic stimulation has shown to provide therapeutic benefits in alleviating symptoms.[205]
Surgery may be used as a last resort in people who do not improve with other treatments. In this procedure, a surgical lesion is made in an area of the brain (the cingulate cortex). In one study, 30% of participants benefitted significantly from this procedure.[206] Deep brain stimulation and vagus nerve stimulation are possible surgical options that do not require destruction of brain tissue. However, because deep brain stimulation results in such an instant and intense change, individuals may experience identity challenges afterward.[207] In the United States, the Food and Drug Administration approved deep-brain stimulation for the treatment of OCD under a humanitarian device exemption, requiring that the procedure be performed only in a hospital with special qualifications to do so.[208]
In the United States, psychosurgery for OCD is a treatment of last resort, and will not be performed until the person has failed several attempts at medication (at the full dosage) with augmentation, and many months of intensive cognitive–behavioral therapy with exposure and ritual/response prevention.[209] Likewise, in the United Kingdom, psychosurgery cannot be performed unless a course of treatment from a suitably qualified cognitive–behavioral therapist has been carried out.
Children
Therapeutic treatment may be effective in reducing ritual behaviors of OCD for children and adolescents.[210] Similar to the treatment of adults with OCD, cognitive behavioral therapy stands as an effective and validated first line of treatment of OCD in children.[211] Family involvement, in the form of behavioral observations and reports, is a key component to the success of such treatments.[212] Parental interventions also provide positive reinforcement for a child who exhibits appropriate behaviors as alternatives to compulsive responses. In a recent meta-analysis of evidenced-based treatment of OCD in children, family-focused individual CBT was labeled as "probably efficacious," establishing it as one of the leading psychosocial treatments for youth with OCD.[211] After one or two years of therapy, in which a child learns the nature of their obsession and acquires strategies for coping, they may acquire a larger circle of friends, exhibit less shyness, and become less self-critical.[213] Trials have shown that children and adolescents with OCD should begin treatment with the combination of CBT with a selective serotonin reuptake inhibitor or CBT alone, rather than only an SSRI.[93][95]
Although the known causes of OCD in younger age groups range from brain abnormalities to psychological preoccupations, life stress such as bullying and traumatic familial deaths may also contribute to childhood cases of OCD, and acknowledging these stressors can play a role in treating the disorder.[214]
Prognosis
Quality of life is reduced across all domains in OCD. While psychological or pharmacological treatment can lead to a reduction of OCD symptoms and an increase in reported quality of life, symptoms may persist at moderate levels even following adequate treatment courses, and completely symptom-free periods are uncommon.[215][216] In pediatric OCD, around 40% still have the disorder in adulthood, and around 40% qualify for remission.[217] The risk of having at least one comorbid personality disorder in OCD is 52%, which is the highest among anxiety disorders and greatly impacts its management and prognosis.[218]
Epidemiology

Obsessive–compulsive disorder affects about 2.3% of people at some point in their life, with the yearly rate about 1.2%.[6] OCD occurs worldwide.[2] It is unusual for symptoms to begin after the age of 35 and half of people develop problems before 20.[1][2] Males and females are affected about equally.[1] However, there is an earlier age for onset for males than females.[219]
History
Plutarch, an ancient Greek philosopher and historian, describes an ancient Roman man who possibly had scrupulosity, which could be a symptom of OCD or OCPD. This man is described as "turning pale under his crown of flowers," praying with a "faltering voice," and scattering "incense with trembling hands."[220][221][222]
In the 7th century AD, John Climacus records an instance of a young monk plagued by constant and overwhelming "temptations to blasphemy" consulting an older monk, who told him: "My son, I take upon myself all the sins which these temptations have led you, or may lead you, to commit. All I require of you is that for the future you pay no attention to them whatsoever."[223]: 212 The Cloud of Unknowing, a Christian mystical text from the late 14th century, recommends dealing with recurring obsessions by attempting to ignore them, and, if that fails, to "cower under them like a poor wretch and a coward overcome in battle, and reckon it to be a waste of your time for you to strive any longer against them", a technique now known as emotional flooding.[223]: 213
Abu Zayd Al-Balkhi, the 9th century Islamic polymath, was likely the first to classify OCD into different types and pioneer cognitive behavioral therapy, in a fashion unique to his era and which was not popular in Greek medicine.[224] In his medical treatise entitled Sustenance of the Body and Soul, Al-Balkhi describes obsessions particular to the disorder as "Annoying thoughts that are not real. These intrusive thoughts prevent enjoying life, and performing daily activities. They affect concentration and interfere with ability to carry out different tasks."[225] As treatment, Al-Balkhi suggests treating obsessive thoughts with positive thoughts and mind-based therapy.[224]
From the 14th to the 16th century in Europe, it was believed that people who experienced blasphemous, sexual or other obsessive thoughts were possessed by the devil.[168][223]: 213 Based on this reasoning, treatment involved banishing the "evil" from the "possessed" person through exorcism.[226][227] The vast majority of people who thought that they were possessed by the devil did not have hallucinations or other "spectacular symptoms" but "complained of anxiety, religious fears, and evil thoughts."[223]: 213 In 1584, a woman from Kent, England, named Mrs. Davie, described by a justice of the peace as "a good wife", was nearly burned at the stake after she confessed that she experienced constant, unwanted urges to murder her family.[223]: 213
The English term obsessive–compulsive arose as a translation of German Zwangsvorstellung (obsession) used in the first conceptions of OCD by Karl Westphal. Westphal's description went on to influence Pierre Janet, who further documented features of OCD.[71] In the early 1910s, Sigmund Freud attributed obsessive–compulsive behavior to unconscious conflicts that manifest as symptoms.[226] Freud describes the clinical history of a typical case of "touching phobia" as starting in early childhood, when the person has a strong desire to touch an item. In response, the person develops an "external prohibition" against this type of touching. However, this "prohibition does not succeed in abolishing" the desire to touch; all it can do is repress the desire and "force it into the unconscious."[228] Freudian psychoanalysis remained the dominant treatment for OCD until the mid-1980s, even though medicinal and therapeutic treatments were known and available, because it was widely thought that these treatments would be detrimental to the effectiveness of the psychotherapy.[223]: 210–211 In the mid-1980s, this approach changed, and practitioners began treating OCD primarily with medicine and practical therapy rather than through psychoanalysis.[223]: 210
One of the first successful treatments of OCD, exposure and response prevention, emerged during the 1960s, when psychologist Vic Meyer exposed two hospitalized patients to anxiety-inducing situations while preventing them from performing any compulsions. Eventually, both patients' anxiety level dropped to manageable levels. Meyer devised this procedure from his analysis of fear extinguishment in animals via flooding.[229] The success of ERP clinically and scientifically has been summarized as "spectacular" by prominent OCD researcher Stanley Rachman decades following Meyer's creation of the method.[230]
In 1967, psychiatrist Juan José López-Ibor reported that the drug clomipramine was effective in treating OCD. Many reports of its success in treatment followed, and several studies had confirmed its effectiveness by the 1980s.[231][232] However, clomipramine was subsequently displaced by new SSRIs developed in the 1970s, such as fluoxetine and sertraline, which were shown to have fewer side effects.[4][232]
Obsessive-compulsive symptoms worsened during the early stages of the COVID-19 pandemic, particularly for individuals with contamination-related OCD.[233]
Notable cases
John Bunyan (1628–1688), the author of The Pilgrim's Progress, displayed symptoms of OCD (which had not yet been named). During the most severe period of his condition, he would mutter the same phrase over and over again to himself while rocking back and forth.[223]: 53–54 He later described his obsessions in his autobiography Grace Abounding to the Chief of Sinners, stating, "These things may seem ridiculous to others, even as ridiculous as they were in themselves, but to me they were the most tormenting cogitations."[223]: 53–54 He wrote two pamphlets advising those with similar anxieties.[223]: 217–218 In one of them, he warns against indulging in compulsions: "Have care of putting off your trouble of spirit in the wrong way: by promising to reform yourself and lead a new life, by your performances or duties".[223]: 217–218
British poet, essayist and lexicographer Samuel Johnson (1709–1784) also had OCD. He had elaborate rituals for crossing the thresholds of doorways, and repeatedly walked up and down staircases counting the steps.[234][223]: 54–55 He would touch every post on the street as he walked past, only step in the middle of paving stones, and repeatedly perform tasks as though they had not been done properly the first time.[223]: 55
The "Rat Man", real name Ernst Lanzer, a patient of Sigmund Freud, suffered from what was then called "obsessional neurosis". Lanzer's illness was characterised most famously by a pattern of distressing intrusive thoughts in which he feared that his father or a female friend would be subjected to a purported Chinese method of torture in which rats would be encouraged to gnaw their way out of a victim's body by a hot poker.[235]
American aviator and filmmaker Howard Hughes is known to have had OCD, primarily an obsessive fear of germs and contamination.[236] Friends of Hughes have also mentioned his obsession with minor flaws in clothing.[237] This was conveyed in The Aviator (2004), a film biography of Hughes.[238]
English singer-songwriter George Ezra has openly spoken about his life-long struggle with OCD, particularly primarily obsessional obsessive–compulsive disorder (Pure O).[239]
Swedish climate activist Greta Thunberg is also known to have OCD, among other mental health conditions.[240]
American actor James Spader has also spoken about his OCD. In 2014, when interviewed for Rolling Stone he said: "I'm obsessive-compulsive. I have very, very strong obsessive-compulsive issues. I'm very particular. ... It's very hard for me, you know? It makes you very addictive in behavior, because routine and ritual become entrenched. But in work, it manifests itself in obsessive attention to detail and fixation. It serves my work very well: Things don't slip by. But I'm not very easygoing.[241]
In 2022 the president of Chile Gabriel Boric stated that he had OCD, saying: "I have an obsessive–compulsive disorder that's completely under control. Thank God I've been able to undergo treatment and it doesn't make me unable to carry out my responsibilities as the President of the Republic."[242]
In a documentary released in 2023, David Beckham shared details about his compelling cleaning rituals, need for symmetry in the fridge, and the impact of OCD on his life.[243]
Society and culture

Art, entertainment and media
Movies and television shows may portray idealized or incomplete representations of disorders such as OCD.[244] Compassionate and accurate literary and on-screen depictions may help counteract the potential stigma associated with an OCD diagnosis, and lead to increased public awareness, understanding and sympathy for such disorders.[245][246]
- The play and film adaptations of The Odd Couple based around the character of Felix, who shows some of the common symptoms of OCD.[247]
- In the film As Good as It Gets (1997), actor Jack Nicholson portrays a man with OCD who performs ritualistic behaviors that disrupt his life.[248]
- The film Matchstick Men (2003) portrays a con man named Roy (Nicolas Cage) with OCD who opens and closes doors three times while counting aloud before he can walk through them.[249]
- In the television series Monk (2002–2009), the titular character Adrian Monk fears both human contact and dirt.[250][251]
- The one-man show The Life and Slimes of Marc Summers (2016), a stage adaptation of Marc Summers' 1999 memoir which recounts how OCD affected his entertainment career.[252]
- In the novel Turtles All the Way Down (2017) by John Green, teenage main character Aza Holmes struggles with OCD that manifests as a fear of the human microbiome. Throughout the story, Aza repeatedly opens an unhealed callus on her finger to drain out what she believes are pathogens. The novel is based on Green's own experiences with OCD. He explained that Turtles All the Way Down is intended to show how "most people with chronic mental illnesses also live long, fulfilling lives".[253]
- The British TV series Pure (2019) stars Charly Clive as a 24-year-old Marnie who is plagued by disturbing sexual thoughts, as a kind of primarily obsessional obsessive compulsive disorder.[254]
Research
The naturally occurring sugar inositol has been suggested as a treatment for OCD.[255]
μ-Opioids agonists, such as hydrocodone and tramadol, may improve OCD symptoms.[256] Administration of opiate treatment may be contraindicated in individuals concurrently taking CYP2D6 inhibitors such as fluoxetine and paroxetine.[257]
Much research is devoted to the therapeutic potential of the agents that affect the release of the neurotransmitter glutamate or the binding to its receptors. These include riluzole, memantine, gabapentin, N-acetylcysteine, topiramate and lamotrigine.[258] Research on the potential for other supplements, such as milk thistle, to help with OCD and various neurological disorders, is ongoing.[259]
Other animals
Advocacy
Many organizations and charities around the world advocate for the wellbeing of people with OCD, stigma reduction, research, and awareness. The International OCD Foundation (IOCDF) is the largest 501(c)3 nonprofit organization dedicated to serving a broad community of individuals with OCD and related disorders, their family members and loved ones, and mental health professionals and researchers around the world. Since 1986, the IOCDF provides up-to-date education and resources, strengthens community engagement worldwide, delivers quality professional training to clinicians, and funds groundbreaking research.
See also
- Anxiety Disorder
- Bipolar disorder
- Body dysmorphic disorder
- Compulsive hoarder
- Cyclothymia
- Delusional disorder
- Hypochondriasis
- Major depressive disorder
- Obsessive–compulsive spectrum
- Tic disorder
- Trichotillomania
References
- ^ a b c d e f g h i j k l m n o p The National Institute of Mental Health (NIMH) (January 2016). "What is Obsessive-Compulsive Disorder (OCD)?". U.S. National Institutes of Health (NIH). Archived from the original on 23 July 2016. Retrieved 24 July 2016.
- ^ a b c d e f g h i j k l m n o p q r s t u v w x Diagnostic and statistical manual of mental disorders: DSM-5 (5th ed.). Washington: American Psychiatric Publishing. 2013. pp. 237–242. ISBN 978-0-89042-555-8.
- ^ a b Angelakis I, Gooding P, Tarrier N, Panagioti M (July 2015). "Suicidality in obsessive compulsive disorder (OCD): a systematic review and meta-analysis". Clinical Psychology Review. 39. Pergamon Press: 1–15. doi:10.1016/j.cpr.2015.03.002. ISSN 0272-7358. PMID 25875222.
- ^ a b c d e f Grant JE (August 2014). "Clinical practice: Obsessive-compulsive disorder". The New England Journal of Medicine. 371 (7): 646–653. doi:10.1056/NEJMcp1402176. PMID 25119610.
- ^ a b c d e Veale D, Miles S, Smallcombe N, Ghezai H, Goldacre B, Hodsoll J (November 2014). "Atypical antipsychotic augmentation in SSRI treatment refractory obsessive-compulsive disorder: a systematic review and meta-analysis". BMC Psychiatry. 14: 317. doi:10.1186/s12888-014-0317-5. PMC 4262998. PMID 25432131.
- ^ a b c Goodman WK, Grice DE, Lapidus KA, Coffey BJ (September 2014). "Obsessive-compulsive disorder". The Psychiatric Clinics of North America. 37 (3): 257–267. doi:10.1016/j.psc.2014.06.004. PMID 25150561.
- ^ a b Sartorius N, Henderson A, Strotzka H, Lipowski Z, Yu-cun S, You-xin X, et al. "The ICD-10 Classification of Mental and Behavioural Disorders Clinical descriptions and diagnostic guidelines" (PDF). who.int World Health Organization. p. 142. Retrieved 8 August 2023.
- ^ a b "Overview – Obsessive compulsive disorder (OCD)". nhs.uk. 16 February 2021. Retrieved 6 November 2021.
- ^ a b c d e "What Is Obsessive-Compulsive Disorder?". psychiatry.org. Retrieved 6 November 2021.
- ^ CDC (2 December 2020). "Obsessive-Compulsive Disorder in Children | CDC". Centers for Disease Control and Prevention. Retrieved 6 November 2021.
- ^ Williams MT, Farris SG, Turkheimer E, Pinto A, Ozanick K, Franklin ME, et al. (June 2011). "Myth of the pure obsessional type in obsessive-compulsive disorder". Depression and Anxiety. 28 (6): 495–500. doi:10.1002/da.20820. PMC 3227121. PMID 21509914.
- ^ "What are compulsions? | OCD-UK". Retrieved 5 November 2021.
- ^ a b Thamby A, Khanna S (2019). "The role of personality disorders in obsessive-compulsive disorder". Indian Journal of Psychiatry. 61 (7): S114–S118. doi:10.4103/psychiatry.IndianJPsychiatry_526_18. PMC 6343421. PMID 30745684.
- ^ Huey ED, Zahn R, Krueger F, Moll J, Kapogiannis D, Wassermann EM, et al. (1 November 2008). "A Psychological and Neuroanatomical Model of Obsessive-Compulsive Disorder". Journal of Neuropsychiatry. 20 (4): 390–408. doi:10.1176/appi.neuropsych.20.4.390. PMC 4476073. PMID 19196924.
- ^ Browne HA, Gair SL, Scharf JM, Grice DE (September 2014). "Genetics of Obsessive-Compulsive Disorder and Related Disorders". Psychiatric Clinics of North America. 37 (3): 319–335. doi:10.1016/j.psc.2014.06.002. PMC 4143777. PMID 25150565.
- ^ a b Starcevic V, Eslick GD, Viswasam K, Berle D (December 2020). "Symptoms of Obsessive-Compulsive Disorder during Pregnancy and the Postpartum Period: a Systematic Review and Meta-Analysis". Psychiatric Quarterly. 91 (4): 965–981. doi:10.1007/s11126-020-09769-8. PMID 32445002. S2CID 218772347.
- ^ a b c Fenske JN, Schwenk TL (August 2009). "Obsessive compulsive disorder: diagnosis and management". American Family Physician. 80 (3): 239–245. PMID 19621834. Archived from the original on 12 May 2014.
- ^ Alonso P, Segalàs C, Real E, Pertusa A, Labad J, Jiménez-Murcia S, et al. (August 2010). "Suicide in patients treated for obsessive-compulsive disorder: a prospective follow-up study". Journal of Affective Disorders. 124 (3): 300–308. doi:10.1016/j.jad.2009.12.001. PMID 20060171.
- ^ Albert U, De Ronchi D, Maina G, Pompili M (25 July 2019). "Suicide Risk in Obsessive-Compulsive Disorder and Exploration of Risk Factors: A Systematic Review". Current Neuropharmacology. 17 (8): 681–696. doi:10.2174/1570159X16666180620155941. PMC 7059158. PMID 29929465.
- ^ Bynum WF, Porter R, Shepherd M (1985). "Obsessional Disorders: A Conceptual History. Terminological and Classificatory Issues.". The anatomy of madness: essays in the history of psychiatry. London: Routledge. pp. 166–187. ISBN 978-0-415-32382-6.
- ^ a b c d "Obsessive-Compulsive Disorder". National Institute of Mental Health (NIMH). Retrieved 23 March 2022.
- ^ "Obsessive-compulsive disorder: MedlinePlus Medical Encyclopedia". medlineplus.gov. Retrieved 25 April 2023.
- ^ "What Is Obsessive-Compulsive Disorder?". American Psychiatric Association. October 2022. Retrieved 25 April 2023.
- ^ a b "Medications Approved for Treatment of OCD". Beyond OCD: OCD Information and Resources. Retrieved 11 December 2021.
- ^ Pittenger C, Bloch MH (September 2014). "Pharmacological treatment of obsessive-compulsive disorder". The Psychiatric Clinics of North America. 37 (3): 375–391. doi:10.1016/j.psc.2014.05.006. PMC 4143776. PMID 25150568.
- ^ a b Gava I, Barbui C, Aguglia E, Carlino D, Churchill R, De Vanna M, et al. (April 2007). "Psychological treatments versus treatment as usual for obsessive compulsive disorder (OCD)". The Cochrane Database of Systematic Reviews (2): CD005333. doi:10.1002/14651858.CD005333.pub2. PMID 17443583.
- ^ a b Bloch MH, McGuire J, Landeros-Weisenberger A, Leckman JF, Pittenger C (August 2010). "Meta-analysis of the dose-response relationship of SSRI in obsessive-compulsive disorder". Molecular Psychiatry. 15 (8): 850–855. doi:10.1038/mp.2009.50. PMC 2888928. PMID 19468281.
- ^ a b Decloedt EH, Stein DJ (May 2010). "Current trends in drug treatment of obsessive-compulsive disorder". Neuropsychiatric Disease and Treatment. 6: 233–242. doi:10.2147/NDT.S3149. PMC 2877605. PMID 20520787.
- ^ Hirschtritt ME, Bloch MH, Mathews CA (4 April 2017). "Obsessive-Compulsive Disorder: Advances in Diagnosis and Treatment". JAMA. 317 (13): 1358–1367. doi:10.1001/jama.2017.2200. PMID 28384832. S2CID 13660201.
- ^ Gadot R, Najera R, Hirani S, Anand A, Storch E, Goodman WK, et al. (November 2022). "Efficacy of deep brain stimulation for treatment-resistant obsessive-compulsive disorder: systematic review and meta-analysis". Journal of Neurology, Neurosurgery & Psychiatry. 93 (11): 1166–1173. doi:10.1136/jnnp-2021-328738. PMID 36127157.
- ^ Fitzsimmons SM, van der Werf YD, van Campen AD, Arns M, Sack AT, Hoogendoorn AW, et al. (April 2022). "Repetitive transcranial magnetic stimulation for obsessive-compulsive disorder: A systematic review and pairwise/network meta-analysis". Journal of Affective Disorders. 302: 302–312. doi:10.1016/j.jad.2022.01.048. hdl:2066/247522. PMID 35041869.
- ^ "Diagnosis and Treatment of Obsessive-Compulsive Disorder in Children and Adolescents (A Systematic Review)". Diagnosis and Treatment of Obsessive-Compulsive Disorder in Children and Adolescents (A Systematic Review) | PCORI. 15 February 2023. Retrieved 28 April 2023.
- ^ "Obsessive Compulsive Disorder". Mercy. Retrieved 24 March 2023.
- ^ Miller ES, Chu C, Gollan J, Gossett DR (March 2013). "Obsessive-compulsive symptoms during the postpartum period. A prospective cohort". The Journal of Reproductive Medicine. 58 (3–4): 115–22. PMC 5705036. PMID 23539879.
- ^ a b Fawcett EJ, Power H, Fawcett JM (23 June 2020). "Women Are at Greater Risk of OCD Than Men: A Meta-Analytic Review of OCD Prevalence Worldwide". The Journal of Clinical Psychiatry. 81 (4). doi:10.4088/JCP.19r13085. PMID 32603559. S2CID 220288984.
- ^ a b Leckman JF, Bloch MH, King RA (2009). "Symptom dimensions and subtypes of obsessive-compulsive disorder: a developmental perspective". Dialogues in Clinical Neuroscience. 11 (1): 21–33. doi:10.31887/DCNS.2009.11.1/jfleckman. PMC 3181902. PMID 19432385.
- ^ Bloch MH, Landeros-Weisenberger A, Rosario MC, Pittenger C, Leckman JF (December 2008). "Meta-analysis of the symptom structure of obsessive-compulsive disorder". The American Journal of Psychiatry. 165 (12): 1532–1542. doi:10.1176/appi.ajp.2008.08020320. PMC 3972003. PMID 18923068.
- ^ a b Swedo SE (1 April 1989). "Obsessive-Compulsive Disorder in Children and Adolescents: Clinical Phenomenology of 70 Consecutive Cases". Archives of General Psychiatry. 46 (4): 335–341. doi:10.1001/archpsyc.1989.01810040041007. PMID 2930330.
- ^ Rasmussen SA, Eisen JL (December 1992). "The epidemiology and clinical features of obsessive compulsive disorder". The Psychiatric Clinics of North America. 15 (4): 743–58. doi:10.1016/S0193-953X(18)30205-3. PMID 1461792.
- ^ Kenyon KM, Eaton WO (16 November 2015). "Age at child obsessive-compulsive disorder onset and its relation to gender, symptom severity, and family functioning". Archives of Scientific Psychology. 3 (1): 150–158. doi:10.1037/arc0000022. hdl:1993/30297.
- ^ a b "About OCD". Obsessive-Compulsive and Related Disorders (in Samoan). Retrieved 13 December 2022.
- ^ McKay D, Abramowitz JS, Calamari JE, Kyrios M, Radomsky A, Sookman D, et al. (July 2004). "A critical evaluation of obsessive-compulsive disorder subtypes: symptoms versus mechanisms". Clinical Psychology Review. 24 (3): 283–313. doi:10.1016/j.cpr.2004.04.003. PMID 15245833.
- ^ Anholt GE, Cath DC, van Oppen P, Eikelenboom M, Smit JH, van Megen H, et al. (May 2010). "Autism and ADHD symptoms in patients with OCD: are they associated with specific OC symptom dimensions or OC symptom severity?". Journal of Autism and Developmental Disorders. 40 (5): 580–589. doi:10.1007/s10803-009-0922-1. PMC 2855859. PMID 20039111.
- ^ Markarian Y, Larson MJ, Aldea MA, Baldwin SA, Good D, Berkeljon A, et al. (February 2010). "Multiple pathways to functional impairment in obsessive-compulsive disorder". Clinical Psychology Review. 30 (1): 78–88. doi:10.1016/j.cpr.2009.09.005. PMID 19853982.
- ^ Doron G, Szepsenwol O, Karp E, Gal N (December 2013). "Obsessing about intimate-relationships: testing the double relationship-vulnerability hypothesis". Journal of Behavior Therapy and Experimental Psychiatry. 44 (4): 433–440. doi:10.1016/j.jbtep.2013.05.003. PMID 23792752.
- ^ Baer L (2001). The Imp of the Mind: Exploring the Silent Epidemic of Obsessive Bad Thoughts. New York: Dutton. p. xiv. ISBN 978-0-525-94562-8.
- ^ Mash EJ, Wolfe DA (2005). Abnormal child psychology (3rd ed.). Belmont, California: Thomson Wadsworth. p. 197. ISBN 978-1-305-10542-3.
- ^ Deacon B, Nelson EA (2008). "On the nature and treatment of scrupulosity" (PDF). Pragmatic Case Studies in Psychotherapy. 4 (2): 39–53. doi:10.14713/pcsp.v4i2.932.
- ^ Huppert JD, Siev J, Kushner ES (October 2007). "When religion and obsessive-compulsive disorder collide: treating scrupulosity in Ultra-Orthodox Jews". Journal of Clinical Psychology. 63 (10): 925–41. doi:10.1002/jclp.20404. PMID 17828763.
- ^ "Mysophobia (Germophobia): Causes, Symptoms & Treatment". Cleveland Clinic. Retrieved 31 March 2023.
- ^ Hammond WA, Morton WJ (1879). Neurological contributions. unknown library. New York, G. P. Putnam's sons.
- ^ a b Osgood-Hynes D. "Thinking Bad Thoughts" (PDF). Belmont, Massachusetts: MGH/McLean OCD Institute. Archived from the original (PDF) on 15 November 2011. Retrieved 30 December 2006.
- ^ Williams M. "Sexual Orientation Worries in Obsessive-Compulsive Disorder". OCD Types. Retrieved 4 February 2021.
- ^ Williams MT, Farris SG (May 2011). "Sexual orientation obsessions in obsessive-compulsive disorder: prevalence and correlates". Psychiatry Research. 187 (1–2). Elsevier: 156–159. doi:10.1016/j.psychres.2010.10.019. PMC 3070770. PMID 21094531.
- ^ Murphy DL, Timpano KR, Wheaton MG, Greenberg BD, Miguel EC (2010). "Obsessive-compulsive disorder and its related disorders: a reappraisal of obsessive-compulsive spectrum concepts". Dialogues in Clinical Neuroscience. 12 (2). Taylor & Francis: 131–148. doi:10.31887/DCNS.2010.12.2/dmurphy. PMC 3181955. PMID 20623919.
- ^ Highlights of Changes from DSM-IV-TR to DSM-5 (PDF), American Psychiatric Association, 2013, p. 7, archived (PDF) from the original on 19 October 2013, retrieved 12 April 2016
- ^ Hermans D, Engelen U, Grouwels L, Joos E, Lemmens J, Pieters G (January 2008). "Cognitive confidence in obsessive-compulsive disorder: distrusting perception, attention and memory". Behaviour Research and Therapy. 46 (1). Elsevier: 98–113. doi:10.1016/j.brat.2007.11.001. PMID 18076865.
- ^ Boyd MA (2007). Psychiatric Nursing: Contemporary Practice. Baltimore, Maryland: Lippincott Williams & Wilkins. ISBN 978-0-397-55178-1.
- ^ Boyd MA (1994). "Integration of Psychosocial Rehabilitation Into Psychiatric Nursing Practice". Issues in Mental Health Nursing. 15 (1): 13–26. doi:10.3109/01612849409074930. PMID 8119793.
- ^ "Obsessive-Compulsive Disorder, (2005)". Retrieved 15 December 2009.
- ^ Storch EA, Stigge-Kaufman D, Marien WE, Sajid M, Jacob ML, Geffken GR, et al. (2008). "Obsessive-compulsive disorder in youth with and without a chronic tic disorder". Depression and Anxiety. 25 (9): 761–767. doi:10.1002/da.20304. PMID 17345600. S2CID 30858531.
- ^ Conelea CA, Walther MR, Freeman JB, Garcia AM, Sapyta J, Khanna M, et al. (December 2014). "Tic-related obsessive-compulsive disorder (OCD): phenomenology and treatment outcome in the Pediatric OCD Treatment Study II". Journal of the American Academy of Child and Adolescent Psychiatry. 53 (12): 1308–1316. doi:10.1016/j.jaac.2014.09.014. PMC 4254546. PMID 25457929.
- ^ "Hygiene of the Skin: When Is Clean Too Clean? Subtopic: "Skin Barrier Properties and Effect of Hand Hygiene Practices", Paragraph 5". Archived from the original on 21 April 2009. Retrieved 26 March 2009.
- ^ Pélissier MC, O'Connor KP (March 2002). "Deductive and inductive reasoning in obsessive-compulsive disorder". The British Journal of Clinical Psychology. 41 (Pt 1). Wiley-Blackwell: 15–27. doi:10.1348/014466502163769. PMID 11931675.
- ^ "Understanding CBT for OCD". Perelman School of Medicine University of Pennsylvania. Retrieved 31 August 2021.
- ^ van den Hout M, Kindt M (June 2004). "Obsessive-compulsive disorder and the paradoxical effects of perseverative behaviour on experienced uncertainty". Journal of Behavior Therapy and Experimental Psychiatry. 35 (2): 165–181. doi:10.1016/j.jbtep.2004.04.007. hdl:1874/11267. PMID 15210377. S2CID 21371127.
- ^ a b Himle MB, Flessner CA, Woods DW (2004). "Advances in the behavior analytic treatment of trichotillomania and Tourette's Syndrome". Journal of Early and Intensive Behavior Intervention. 1 (1): 57–64. doi:10.1037/h0100282. ISSN 1554-4893.
- ^ a b Sarris J, Camfield D, Berk M (May 2012). "Complementary medicine, self-help, and lifestyle interventions for obsessive compulsive disorder (OCD) and the OCD spectrum: a systematic review". Journal of Affective Disorders. 138 (3): 213–221. doi:10.1016/j.jad.2011.04.051. PMID 21620478.
- ^ Weisman MM (May 1998). "The cross national epidemiology of obsessive–compulsive disorder". New Developments in Obsessive-Compulsive and Spectrum Disorders. 3 (1): 6–9.
- ^ Substance Abuse and Mental Health Services Administration (June 2016). "Table 3.13, DSM-IV to DSM-5 Obsessive-Compulsive Disorder Comparison". Impact of the DSM-IV to DSM-5 Changes on the National Survey on Drug Use and Health [Internet]. Retrieved 11 December 2021.
- ^ a b Ruiz P, Sadock B, Sadock V (2017). Kaplan and Sadock's Comprehensive Textbook of Psychiatry (10th ed.). LWW. ISBN 978-1-4511-0047-1.
- ^ O'Dwyer AM, Marks I (March 2000). "Obsessive-compulsive disorder and delusions revisited". The British Journal of Psychiatry: The Journal of Mental Science. 176 (3): 281–4. doi:10.1192/bjp.176.3.281. PMID 10755077. S2CID 8365071.
- ^ a b Veale D (April 2002). "Over-valued ideas: a conceptual analysis". Behaviour Research and Therapy. 40 (4): 383–400. doi:10.1016/S0005-7967(01)00016-X. PMID 12002896.
- ^ Kozak MJ, Foa EB (1994). "Obsessions, overvalued ideas, and delusions in obsessive-compulsive disorder". Behaviour Research and Therapy. 32 (3): 343–353. doi:10.1016/0005-7967(94)90132-5. ISSN 0005-7967. PMID 8192634.
- ^ Veale D (2002). "Over-valuedideas: aconceptualanalysis" (PDF). Behaviour Research and Therapy (40): 1.
- ^ a b Borda T, Neziroglu F, Taboas W, McKay D, Frenkiel L (September 2017). "Overvalued ideation in adolescents with obsessive-compulsive disorder". Psychiatry Research. 255: 66–71. doi:10.1016/j.psychres.2017.05.001. PMID 28528243. S2CID 4627755.
- ^ Kozak MJ, Foa EB (March 1994). "Obsessions, overvalued ideas, and delusions in obsessive-compulsive disorder". Behaviour Research and Therapy. 32 (3): 343–353. doi:10.1016/0005-7967(94)90132-5. PMID 8192634.
- ^ Neziroglu F, McKay D, Yaryura-Tobias JA, Stevens KP, Todaro J (September 1999). "The Overvalued Ideas Scale: development, reliability and validity in obsessive-compulsive disorder". Behaviour Research and Therapy. 37 (9): 881–902. doi:10.1016/S0005-7967(98)00191-0. PMID 10458051.
- ^ Abramovitch A, Anholt G, Raveh-Gottfried S, Hamo N, Abramowitz JS (March 2018). "Meta-Analysis of Intelligence Quotient (IQ) in Obsessive-Compulsive Disorder". Neuropsychology Review. 28 (1): 111–120. doi:10.1007/s11065-017-9358-0. PMID 28864868. S2CID 4012128.
- ^ Shin NY, Lee TY, Kim E, Kwon JS (April 2014). "Cognitive functioning in obsessive-compulsive disorder: a meta-analysis". Psychological Medicine. 44 (6): 1121–1130. doi:10.1017/S0033291713001803. PMID 23866289. S2CID 28181106.
- ^ Çetinay Aydın P, Güleç Öyekçin D (2013). "[Cognitive functions in patients with obsessive compulsive disorder]". Turk Psikiyatri Dergisi = Turkish Journal of Psychiatry. 24 (4): 266–274. doi:10.5080/u7172. PMID 24310094.
- ^ Pauls DL, Abramovitch A, Rauch SL, Geller DA (June 2014). "Obsessive-compulsive disorder: an integrative genetic and neurobiological perspective". Nature Reviews. Neuroscience. 15 (6): 410–424. doi:10.1038/nrn3746. PMID 24840803. S2CID 17781028.
- ^ Leopold R, Backenstrass M (March 2015). "Neuropsychological differences between obsessive-compulsive washers and checkers: a systematic review and meta-analysis". Journal of Anxiety Disorders. 30: 48–58. doi:10.1016/j.janxdis.2014.12.016. PMID 25601381.
- ^ Abramovitch A, Cooperman A (April 2015). "The cognitive neuropsychology of obsessive-compulsive disorder: A critical review". Journal of Obsessive-Compulsive and Related Disorders. 5: 24–36. doi:10.1016/j.jocrd.2015.01.002.
- ^ González-Bueso V, Santamaría JJ, Fernández D, Merino L, Montero E, Ribas J (2018). "Association between Internet Gaming Disorder or Pathological Video-Game Use and Comorbid Psychopathology: A Comprehensive Review". International Journal of Environmental Research and Public Health. 15 (4). MDPI: 668. doi:10.3390/ijerph15040668. PMC 5923710. PMID 29614059.
- ^ Jones AM, De Nadai AS, Arnold EB, McGuire JF, Lewin AB, Murphy TK, et al. (February 2013). "Psychometric properties of the obsessive compulsive inventory: child version in children and adolescents with obsessive-compulsive disorder". Child Psychiatry and Human Development. 44 (1): 137–151. doi:10.1007/s10578-012-0315-0. PMID 22711294. S2CID 27470036.
- ^ Blanco-Vieira T, Radua J, Marcelino L, Bloch M, Mataix-Cols D, do Rosário MC (28 June 2023). "The genetic epidemiology of obsessive-compulsive disorder: a systematic review and meta-analysis". Translational Psychiatry. 13 (1): 230. doi:10.1038/s41398-023-02433-2. PMC 10307810. PMID 37380645.
- ^ Last CG, Strauss CC (1989). "Obsessive—compulsive disorder in childhood". Journal of Anxiety Disorders. 3 (4): 295–302. doi:10.1016/0887-6185(89)90020-0.
- ^ a b c Rapp AM, Bergman RL, Piacentini J, Mcguire JF (January 2016). "Evidence-Based Assessment of Obsessive–Compulsive Disorder". Journal of Central Nervous System Disease. 8: 13–29. doi:10.4137/JCNSD.S38359. PMC 4994744. PMID 27594793.
- ^ McGuire JF, Piacentini J, Lewin AB, Brennan EA, Murphy TK, Storch EA (August 2015). "A Meta-analysis of Cognitive Behavior Therapy and Medication for Child Obsessive-compulsive Disorder: Moderators of Treatment Efficacy, Response, and Remission: Research Article: Treatment Outcomes and Moderators in Pediatric OCD". Depression and Anxiety. 32 (8): 580–593. doi:10.1002/da.22389. PMC 4515191. PMID 26130211.
- ^ McGuire JF, Lewin AB, Horng B, Murphy TK, Storch EA (January 2012). "The Nature, Assessment, and Treatment of Obsessive–Compulsive Disorder". Postgraduate Medicine. 124 (1): 152–165. doi:10.3810/pgm.2012.01.2528. PMID 22314125. S2CID 207639773.
- ^ Watson HJ, Rees CS (May 2008). "Meta-analysis of randomized, controlled treatment trials for pediatric obsessive-compulsive disorder". Journal of Child Psychology and Psychiatry. 49 (5): 489–498. doi:10.1111/j.1469-7610.2007.01875.x. PMID 18400058.
- ^ a b Pediatric OCD Treatment Study (POTS) Team (27 October 2004). "Cognitive-Behavior Therapy, Sertraline, and Their Combination for Children and Adolescents With Obsessive-Compulsive Disorder: The Pediatric OCD Treatment Study (POTS) Randomized Controlled Trial". JAMA. 292 (16): 1969–1976. doi:10.1001/jama.292.16.1969. PMID 15507582.
- ^ Geller DA, Biederman J, Stewart SE, Mullin B, Martin A, Spencer T, et al. (November 2003). "Which SSRI? A Meta-Analysis of Pharmacotherapy Trials in Pediatric Obsessive-Compulsive Disorder". American Journal of Psychiatry. 160 (11): 1919–1928. doi:10.1176/appi.ajp.160.11.1919. PMID 14594734. S2CID 8711232.
- ^ a b Geller DA, March J (January 2012). "Practice Parameter for the Assessment and Treatment of Children and Adolescents With Obsessive-Compulsive Disorder". Journal of the American Academy of Child & Adolescent Psychiatry. 51 (1): 98–113. doi:10.1016/j.jaac.2011.09.019. PMID 22176943.
- ^ Chen YW, Dilsaver SC (November 1995). "Comorbidity for obsessive-compulsive disorder in bipolar and unipolar disorders". Psychiatry Research. 59 (1–2): 57–64. doi:10.1016/0165-1781(95)02752-1. PMID 8771221. S2CID 2782199.
- ^ Angelakis I, Gooding P, Tarrier N, Panagioti M (July 2015). "Suicidality in obsessive compulsive disorder (OCD): a systematic review and meta-analysis". Clinical Psychology Review. 39: 1–15. doi:10.1016/j.cpr.2015.03.002. PMID 25875222.
- ^ a b Bang L, Kristensen UB, Wisting L, Stedal K, Garte M, Minde Å, et al. (January 2020). "Presence of eating disorder symptoms in patients with obsessive-compulsive disorder". BMC Psychiatry. 20 (1): 36. doi:10.1186/s12888-020-2457-0. PMC 6993325. PMID 32000754.
- ^ Tyagi H, Patel R, Rughooputh F, Abrahams H, Watson AJ, Drummond L (2015). "Comparative Prevalence of Eating Disorders in Obsessive-Compulsive Disorder and Other Anxiety Disorders". Psychiatry Journal. 2015. Hindawi Psychiatry Journal: 186927. doi:10.1155/2015/186927. PMC 4561118. PMID 26366407.
- ^ Turner J, Drummond LM, Mukhopadhyay S, Ghodse H, White S, Pillay A, et al. (June 2007). "A prospective study of delayed sleep phase syndrome in patients with severe resistant obsessive-compulsive disorder". World Psychiatry. 6 (2): 108–111. PMC 2219909. PMID 18235868.
- ^ a b Paterson JL, Reynolds AC, Ferguson SA, Dawson D (December 2013). "Sleep and obsessive-compulsive disorder (OCD)". Sleep Medicine Reviews. 17 (6): 465–474. doi:10.1016/j.smrv.2012.12.002. PMID 23499210.
- ^ Mineka S, Watson D, Clark LA (1998). "Comorbidity of anxiety and unipolar mood disorders". Annual Review of Psychology. 49: 377–412. doi:10.1146/annurev.psych.49.1.377. PMID 9496627. S2CID 14546782.
- ^ Pediatric Obsessive-Compulsive Disorder Differential Diagnoses Archived 17 September 2012 at the Wayback Machine – 2012
- ^ Mansueto CS, Keuler DJ (September 2005). "Tic or compulsion?: it's Tourettic OCD". Behavior Modification. 29 (5): 784–799. doi:10.1177/0145445505279261. PMID 16046664. S2CID 146592937.
- ^ "OCD and Tourette Syndrome: Re-examining the Relationship". International OCD Foundation. Archived from the original on 1 November 2013. Retrieved 30 October 2013.
- ^ Pallanti S, Grassi G, Sarrecchia ED, Cantisani A, Pellegrini M (2011). "Obsessive-compulsive disorder comorbidity: clinical assessment and therapeutic implications". Frontiers in Psychiatry. 2: 70. doi:10.3389/fpsyt.2011.00070. PMC 3243905. PMID 22203806.
- ^ Ou W, Li Z, Zheng Q, Chen W, Liu J, Liu B, et al. (20 January 2021). "Association Between Childhood Maltreatment and Symptoms of Obsessive-Compulsive Disorder: A Meta-Analysis". Frontiers in Psychiatry. 11: 612586. doi:10.3389/fpsyt.2020.612586. PMC 7854900. PMID 33551875.
- ^ Gu W, Zhao Q, Yuan C, Yi Z, Zhao M, Wang Z (2022). "Impact of adverse childhood experiences on the symptom severity of different mental disorders: a cross-diagnostic study". General Psychiatry. 35 (2): e100741. doi:10.1136/gpsych-2021-100741. PMC 9036421. PMID 35572774.
- ^ Alevizos B, Papageorgiou C, Christodoulou GN (September 2004). "Obsessive-compulsive symptoms with olanzapine". The International Journal of Neuropsychopharmacology. 7 (3): 375–377. doi:10.1017/S1461145704004456. PMID 15231024.
- ^ Kulkarni G, Narayanaswamy JC, Math SB (1 January 2012). "Olanzapine induced de-novo obsessive compulsive disorder in a patient with schizophrenia". Indian Journal of Pharmacology. 44 (5): 649–650. doi:10.4103/0253-7613.100406. PMC 3480803. PMID 23112432.
- ^ Lykouras L, Zervas IM, Gournellis R, Malliori M, Rabavilas A (September 2000). "Olanzapine and obsessive-compulsive symptoms". European Neuropsychopharmacology. 10 (5): 385–387. doi:10.1016/s0924-977x(00)00096-1. PMID 10974610. S2CID 276209.
- ^ Schirmbeck F, Zink M (March 2012). "Clozapine-induced obsessive-compulsive symptoms in schizophrenia: a critical review". Current Neuropharmacology. 10 (1): 88–95. doi:10.2174/157015912799362724. PMC 3286851. PMID 22942882.
- ^ "Substance/Medication-Induced Obsessive-Compulsive and related disorder". PsychDB. 2 February 2022. Retrieved 28 February 2024.
- ^ Abramowitz JS, Taylor S, McKay D (August 2009). "Obsessive-compulsive disorder". Lancet. 374 (9688): 491–499. doi:10.1016/S0140-6736(09)60240-3. PMID 19665647. S2CID 203833429.
- ^ Menzies L, Achard S, Chamberlain SR, Fineberg N, Chen CH, del Campo N, et al. (December 2007). "Neurocognitive endophenotypes of obsessive-compulsive disorder". Brain. 130 (Pt 12): 3223–3236. doi:10.1093/brain/awm205. PMID 17855376.
- ^ a b Lee EB, Barney JL, Twohig MP, Lensegrav-Benson T, Quakenbush B (April 2020). "Obsessive compulsive disorder and thought action fusion: Relationships with eating disorder outcomes". Eating Behaviors. 37: 101386. doi:10.1016/j.eatbeh.2020.101386. PMID 32388080. S2CID 218585620.
- ^ Levinson CA, Brosof LC, Ram SS, Pruitt A, Russell S, Lenze EJ (August 2019). "Obsessions are strongly related to eating disorder symptoms in anorexia nervosa and atypical anorexia nervosa". Eating Behaviors. 34: 101298. doi:10.1016/j.eatbeh.2019.05.001. PMC 6708491. PMID 31176948.
- ^ Meier M, Kossakowski JJ, Jones PJ, Kay B, Riemann BC, McNally RJ (March 2020). "Obsessive-compulsive symptoms in eating disorders: A network investigation". The International Journal of Eating Disorders. 53 (3): 362–371. doi:10.1002/eat.23196. PMID 31749199. S2CID 208214719.
- ^ Ozaki N, Goldman D, Kaye WH, Plotnicov K, Greenberg BD, Lappalainen J, et al. (November 2003). "Serotonin transporter missense mutation associated with a complex neuropsychiatric phenotype". Molecular Psychiatry. 8 (11): 933–936. doi:10.1038/sj.mp.4001365. PMID 14593431. S2CID 2171955.
- ^ Bloch MH, Landeros-Weisenberger A, Sen S, Dombrowski P, Kelmendi B, Coric V, et al. (September 2008). "Association of the serotonin transporter polymorphism and obsessive-compulsive disorder: systematic review". American Journal of Medical Genetics. Part B, Neuropsychiatric Genetics. 147B (6): 850–858. doi:10.1002/ajmg.b.30699. PMID 18186076. S2CID 23223447.
- ^ Lin PY (April 2007). "Meta-analysis of the association of serotonin transporter gene polymorphism with obsessive-compulsive disorder". Progress in Neuro-Psychopharmacology & Biological Psychiatry. 31 (3): 683–689. doi:10.1016/j.pnpbp.2006.12.024. PMID 17291658. S2CID 40442832.
- ^ Stewart SE, Yu D, Scharf JM, Neale BM, Fagerness JA, Mathews CA, et al. (July 2013). "Genome-wide association study of obsessive-compulsive disorder". Molecular Psychiatry. 18 (7): 788–798. doi:10.1038/mp.2012.85. PMC 4218751. PMID 22889921.
- ^ Stewart SE, Mayerfeld C, Arnold PD, Crane JR, O'Dushlaine C, Fagerness JA, et al. (June 2013). "Meta-analysis of association between obsessive-compulsive disorder and the 3' region of neuronal glutamate transporter gene SLC1A1". American Journal of Medical Genetics. Part B, Neuropsychiatric Genetics. 162B (4): 367–379. doi:10.1002/ajmg.b.32137. hdl:2027.42/98412. PMID 23606572. S2CID 20929721.
- ^ Pooley EC, Fineberg N, Harrison PJ (June 2007). "The met(158) allele of catechol-O-methyltransferase (COMT) is associated with obsessive-compulsive disorder in men: case-control study and meta-analysis". Molecular Psychiatry. 12 (6): 556–561. doi:10.1038/sj.mp.4001951. PMID 17264842. S2CID 12532617.
- ^ Azzam A, Mathews CA (November 2003). "Meta-analysis of the association between the catecholamine-O-methyl-transferase gene and obsessive-compulsive disorder". American Journal of Medical Genetics. Part B, Neuropsychiatric Genetics. 123B (1): 64–69. doi:10.1002/ajmg.b.20013. PMID 14582147. S2CID 42840925.
- ^ Bracha HS (July 2006). "Human brain evolution and the "Neuroevolutionary Time-depth Principle:" Implications for the Reclassification of fear-circuitry-related traits in DSM-V and for studying resilience to warzone-related posttraumatic stress disorder". Progress in Neuro-Psychopharmacology & Biological Psychiatry. 30 (5): 827–853. doi:10.1016/j.pnpbp.2006.01.008. PMC 7130737. PMID 16563589.
- ^ a b "Overview - Obsessive compulsive disorder (OCD)". nhs.uk. 16 February 2021. Retrieved 23 March 2022.
- ^ "Obsessive-compulsive Disorder | NAMI: National Alliance on Mental Illness". www.nami.org. Retrieved 23 March 2022.
- ^ a b "How SSRIs work | OCD-UK". Retrieved 23 March 2022.
- ^ Sigra S, Hesselmark E, Bejerot S (March 2018). "Treatment of PANDAS and PANS: a systematic review". Neuroscience and Biobehavioral Reviews. 86: 51–65. doi:10.1016/j.neubiorev.2018.01.001. PMID 29309797. S2CID 40827012.
- ^ Wilbur C, Bitnun A, Kronenberg S, Laxer RM, Levy DM, Logan WJ, et al. (May 2019). "PANDAS/PANS in childhood: Controversies and evidence". Paediatrics & Child Health. 24 (2): 85–91. doi:10.1093/pch/pxy145. PMC 6462125. PMID 30996598.
- ^ Boileau B (2011). "A review of obsessive-compulsive disorder in children and adolescents". Dialogues in Clinical Neuroscience. 13 (4): 401–411. doi:10.31887/DCNS.2011.13.4/bboileau. PMC 3263388. PMID 22275846.
- ^ a b Dale RC (December 2017). "Tics and Tourette: a clinical, pathophysiological and etiological review". Current Opinion in Pediatrics (Review). 29 (6): 665–673. doi:10.1097/MOP.0000000000000546. PMID 28915150. S2CID 13654194.
- ^ a b c d Marazziti D, Mucci F, Fontenelle LF (July 2018). "Immune system and obsessive-compulsive disorder". Psychoneuroendocrinology (Review). 93: 39–44. doi:10.1016/j.psyneuen.2018.04.013. PMID 29689421. S2CID 13681480.
- ^ a b c d Zibordi F, Zorzi G, Carecchio M, Nardocci N (March 2018). "CANS: Childhood acute neuropsychiatric syndromes". European Journal of Paediatric Neurology (Review). 22 (2): 316–320. doi:10.1016/j.ejpn.2018.01.011. PMID 29398245.
- ^ Shulman ST (February 2009). "Pediatric autoimmune neuropsychiatric disorders associated with streptococci (PANDAS): update". Current Opinion in Pediatrics. 21 (1): 127–130. doi:10.1097/MOP.0b013e32831db2c4. PMID 19242249. S2CID 37434919.
Despite continued research in the field, the relationship between GAS and specific neuropsychiatric disorders (PANDAS) remains elusive.
- ^ Maia TV, Cooney RE, Peterson BS (2008). "The neural bases of obsessive-compulsive disorder in children and adults". Development and Psychopathology. 20 (4): 1251–1283. doi:10.1017/S0954579408000606. PMC 3079445. PMID 18838041.
- ^ Robertson MM (February 2011). "Gilles de la Tourette syndrome: the complexities of phenotype and treatment". British Journal of Hospital Medicine. 72 (2): 100–107. doi:10.12968/hmed.2011.72.2.100. PMID 21378617.
- ^ Singer HS (2011). "Tourette syndrome and other tic disorders". Hyperkinetic Movement Disorders. Handbook of Clinical Neurology. Vol. 100. pp. 641–57. doi:10.1016/B978-0-444-52014-2.00046-X. ISBN 978-0-444-52014-2. PMID 21496613.
- ^ Pearlman DM, Vora HS, Marquis BG, Najjar S, Dudley LA (July 2014). "Anti-basal ganglia antibodies in primary obsessive-compulsive disorder: systematic review and meta-analysis". The British Journal of Psychiatry. 205 (1): 8–16. doi:10.1192/bjp.bp.113.137018. PMID 24986387.
- ^ Rotge JY, Guehl D, Dilharreguy B, Cuny E, Tignol J, Bioulac B, et al. (September 2008). "Provocation of obsessive-compulsive symptoms: a quantitative voxel-based meta-analysis of functional neuroimaging studies". Journal of Psychiatry & Neuroscience. 33 (5): 405–412. PMC 2527721. PMID 18787662.
- ^ Whiteside SP, Port JD, Abramowitz JS (November 2004). "A meta-analysis of functional neuroimaging in obsessive-compulsive disorder". Psychiatry Research. 132 (1): 69–79. doi:10.1016/j.pscychresns.2004.07.001. PMID 15546704. S2CID 9941792.
- ^ Rasgon A, Lee WH, Leibu E, Laird A, Glahn D, Goodman W, et al. (October 2017). "Neural correlates of affective and non-affective cognition in obsessive compulsive disorder: A meta-analysis of functional imaging studies". European Psychiatry. 46: 25–32. doi:10.1016/j.eurpsy.2017.08.001. PMID 28992533. S2CID 5368803.
- ^ Brem S, Grünblatt E, Drechsler R, Riederer P, Walitza S (September 2014). "The neurobiological link between OCD and ADHD". Attention Deficit and Hyperactivity Disorders. 6 (3): 175–202. doi:10.1007/s12402-014-0146-x. PMC 4148591. PMID 25017045.
- ^ a b c Radua J, van den Heuvel OA, Surguladze S, Mataix-Cols D (July 2010). "Meta-analytical comparison of voxel-based morphometry studies in obsessive-compulsive disorder vs other anxiety disorders". Archives of General Psychiatry. 67 (7): 701–711. doi:10.1001/archgenpsychiatry.2010.70. PMID 20603451. S2CID 9501322.
- ^ Piras F, Piras F, Chiapponi C, Girardi P, Caltagirone C, Spalletta G (January 2015). "Widespread structural brain changes in OCD: a systematic review of voxel-based morphometry studies". Cortex; A Journal Devoted to the Study of the Nervous System and Behavior. 62: 89–108. doi:10.1016/j.cortex.2013.01.016. PMID 23582297. S2CID 206984783.
- ^ Radua J, Mataix-Cols D (November 2009). "Voxel-wise meta-analysis of grey matter changes in obsessive-compulsive disorder". The British Journal of Psychiatry. 195 (5): 393–402. doi:10.1192/bjp.bp.108.055046. PMID 19880927.
- ^ Radua J, Grau M, van den Heuvel OA, Thiebaut de Schotten M, Stein DJ, Canales-Rodríguez EJ, et al. (June 2014). "Multimodal voxel-based meta-analysis of white matter abnormalities in obsessive-compulsive disorder". Neuropsychopharmacology. 39 (7): 1547–1557. doi:10.1038/npp.2014.5. PMC 4023155. PMID 24407265.
- ^ Friedlander L, Desrocher M (January 2006). "Neuroimaging studies of obsessive-compulsive disorder in adults and children". Clinical Psychology Review. 26 (1): 32–49. doi:10.1016/j.cpr.2005.06.010. PMID 16242823.
- ^ Stern ER, Taylor SF (September 2014). "Cognitive neuroscience of obsessive-compulsive disorder". The Psychiatric Clinics of North America. 37 (3): 337–352. doi:10.1016/j.psc.2014.05.004. PMID 25150566. S2CID 207442722.
- ^ a b Wood J, Ahmari SE (2015). "A Framework for Understanding the Emerging Role of Corticolimbic-Ventral Striatal Networks in OCD-Associated Repetitive Behaviors". Frontiers in Systems Neuroscience. 9: 171. doi:10.3389/fnsys.2015.00171. PMC 4681810. PMID 26733823.
- ^ Nakao T, Okada K, Kanba S (August 2014). "Neurobiological model of obsessive-compulsive disorder: evidence from recent neuropsychological and neuroimaging findings". Psychiatry and Clinical Neurosciences. 68 (8): 587–605. doi:10.1111/pcn.12195. PMID 24762196. S2CID 5528241.
- ^ Barahona-Corrêa JB, Camacho M, Castro-Rodrigues P, Costa R, Oliveira-Maia AJ (2015). "From Thought to Action: How the Interplay Between Neuroscience and Phenomenology Changed Our Understanding of Obsessive-Compulsive Disorder". Frontiers in Psychology. 6: 1798. doi:10.3389/fpsyg.2015.01798. PMC 4655583. PMID 26635696.
- ^ Davis KL (2002). Neuropsychopharmacology: the fifth generation of progress: an official publication of the American College of Neuropsychopharmacology (5th ed.). Philadelphia, Pa.: Lippincott Williams & Wilkins. pp. 1609–1610. ISBN 978-0-7817-2837-9.
- ^ Muller CP, Jacobs BL, Dijk A, Klompmakers A, Deny D (2009). "4.4 The Serotonergic System in Obsessive-Compulsive Disorder". Handbook of the behavioral neurobiology of serotonin s (1st ed.). London: Academic. pp. 547–558. ISBN 978-0-12-374634-4.
- ^ Kim KW, Lee DY (2002). "Obsessive-compulsive disorder associated with a left orbitofrontal infarct". The Journal of Neuropsychiatry and Clinical Neurosciences. 14 (1): 88–89. doi:10.1176/appi.neuropsych.14.1.88. PMID 11884667.
- ^ Wood J, Ahmari SE (17 December 2015). "A Framework for Understanding the Emerging Role of Corticolimbic-Ventral Striatal Networks in OCD-Associated Repetitive Behaviors". Frontiers in Systems Neuroscience. 9: 171. doi:10.3389/fnsys.2015.00171. PMC 4681810. PMID 26733823.
- ^ a b Pittenger C, Bloch MH, Williams K (December 2011). "Glutamate abnormalities in obsessive compulsive disorder: neurobiology, pathophysiology, and treatment". Pharmacology & Therapeutics. 132 (3): 314–332. doi:10.1016/j.pharmthera.2011.09.006. PMC 3205262. PMID 21963369.
- ^ Graat I, Figee M, Denys D. "Neurotransmitter Dysregulation in OCD". In Pittinger C (ed.). Obsessive-Compulsive Disorder: Phenomenology, Pathophysiology and Treatment. Oxford University Press.
- ^ Aoki Y, Aoki A, Suwa H (August 2012). "Reduction of N-acetylaspartate in the medial prefrontal cortex correlated with symptom severity in obsessive-compulsive disorder: meta-analyses of (1)H-MRS studies". Translational Psychiatry. 2 (8): e153. doi:10.1038/tp.2012.78. PMC 3432192. PMID 22892718.
- ^ a b Quick Reference to the Diagnostic Criteria from DSM-IV-TR. Arlington, VA: American Psychiatric Association, 2000.
- ^ Goodman WK, Price LH, Rasmussen SA, Mazure C, Fleischmann RL, Hill CL, et al. (November 1989). "The Yale-Brown Obsessive Compulsive Scale. I. Development, use, and reliability". Archives of General Psychiatry. 46 (11): 1006–1011. doi:10.1001/archpsyc.1989.01810110048007. PMID 2684084.
- ^ Foa EB, Huppert JD, Leiberg S, Langner R, Kichic R, Hajcak G, et al. (December 2002). "The Obsessive-Compulsive Inventory: development and validation of a short version". Psychological Assessment. 14 (4): 485–496. doi:10.1037/1040-3590.14.4.485. PMID 12501574. S2CID 18815147.
- ^ a b c "Obsessive Compulsive Disorder (OCD): Symptoms & Treatment". Cleveland Clinic. Retrieved 12 October 2022.
- ^ Starcevic V, Janca A (January 2011). "Obsessive-compulsive spectrum disorders: still in search of the concept-affirming boundaries". Current Opinion in Psychiatry. 24 (1): 55–60. doi:10.1097/yco.0b013e32833f3b58. PMID 20827198. S2CID 41312244.
- ^ Freckelton I (June 2020). "Obsessive compulsive disorder and obsessive compulsive personality disorder and the criminal law". Psychiatry, Psychology and Law. 27 (5): 831–852. doi:10.1080/13218719.2020.1745497. PMC 8009125. PMID 33833612.
- ^ Hezel D (January 2022). "Delay to diagnosis in OCD". Journal of Obsessive-Compulsive and Related Disorders. 32: 100709. doi:10.1016/j.jocrd.2022.100709. S2CID 245996392.
- ^ a b Aardema F, O'Connor K (2007). "The menace within: obsessions and the self". Journal of Cognitive Psychotherapy. 21 (3): 182–197. doi:10.1891/088983907781494573. S2CID 143731458.
- ^ Aardema F, O'Connor K (2003). "Seeing white bears that are not there: Inference processes in obsessions". Journal of Cognitive Psychotherapy. 17: 23–37. doi:10.1891/jcop.17.1.23.58270. S2CID 143040967.
- ^ a b Carter, K. "Obsessive–compulsive personality disorder." PSYC 210 lecture: Oxford College of Emory University. Oxford, GA. 11 April 2006.
- ^ a b National Institute for Health and Clinical Excellence (NICE) (November 2005). "Obsessive-compulsive disorder: Core interventions in the treatment of obsessive-compulsive disorder and body dysmorphic disorder". Information about NICE Clinical Guideline 31. UK National Health Service (NHS). Archived from the original on 12 January 2017. Retrieved 24 July 2016.
- ^ Imai H, Tajika A, Narita H, Yoshinaga N, Kimura K, Nakamura H, et al. (April 2022). "Unguided Computer-Assisted Self-Help Interventions Without Human Contact in Patients With Obsessive-Compulsive Disorder: Systematic Review and Meta-analysis". Journal of Medical Internet Research. 24 (4): e35940. doi:10.2196/35940. PMC 9073609. PMID 35451993.
- ^ van Loenen I, Scholten W, Muntingh A, Smit J, Batelaan N (February 2022). "The Effectiveness of Virtual Reality Exposure-Based Cognitive Behavioral Therapy for Severe Anxiety Disorders, Obsessive-Compulsive Disorder, and Posttraumatic Stress Disorder: Meta-analysis". Journal of Medical Internet Research. 24 (2): e26736. doi:10.2196/26736. PMC 8874794. PMID 35142632.
- ^ a b Huppert & Roth: (2003) Treating Obsessive-Compulsive Disorder with Exposure and Response Prevention. The Behavior Analyst Today, 4 (1), 66 – 70 BAO Archived 23 March 2010 at the Wayback Machine
- ^ Klein DF (August 2000). "Flawed meta-analyses comparing psychotherapy with pharmacotherapy". The American Journal of Psychiatry. 157 (8): 1204–1211. doi:10.1176/appi.ajp.157.8.1204. PMID 10910778.
- ^ Fisher PL, Cherry MG, Stuart T, Rigby JW, Temple J (1 October 2020). "People with obsessive-compulsive disorder often remain symptomatic following psychological treatment: A clinical significance analysis of manualised psychological interventions". Journal of Affective Disorders. 275: 94–108. doi:10.1016/j.jad.2020.06.019. ISSN 0165-0327. PMID 32658831. S2CID 220521468.
- ^ Schneider SC, Knott L, Cepeda SL, Hana LM, McIngvale E, Goodman WK, et al. (May 2020). "Serious negative consequences associated with exposure and response prevention for obsessive-compulsive disorder: A survey of therapist attitudes and experiences". Depression and Anxiety. 37 (5): 418–428. doi:10.1002/da.23000. ISSN 1091-4269. PMID 32048376. S2CID 211085261.
- ^ Jalal B, Chamberlain S, Robbins T, Sahakian B (2022). "Obsessive-compulsive disorder-contamination fears, features, and treatment:novel smartphone therapies in light of global mental health and pandemics (COVID-19)". CNS Spectrums. 27 (2): 138. doi:10.1017/S1092852920001947. PMC 7691644. PMID 33081864. Retrieved 29 February 2024.
- ^ Twohig MP, Hayes SC, Masuda A (March 2006). "Increasing willingness to experience obsessions: acceptance and commitment therapy as a treatment for obsessive-compulsive disorder". Behavior Therapy. 37 (1): 3–13. doi:10.1016/j.beth.2005.02.001. PMID 16942956.
- ^ Twohig MP, Abramowitz JS, Bluett EJ, Fabricant LE, Jacoby RJ, Morrison KL, et al. (1 July 2015). "Exposure therapy for OCD from an acceptance and commitment therapy (ACT) framework". Journal of Obsessive-Compulsive and Related Disorders. 6: 167–173. doi:10.1016/j.jocrd.2014.12.007. ISSN 2211-3649.
- ^ Hayes SC. "ACT | Association for Contextual Behavioral Science". contextualscience.org. Retrieved 7 July 2022.
- ^ Hayes SC, Strosahl K, Wilson KG (2012). Acceptance and commitment therapy: the process and practice of mindful change (2nd ed.). New York: Guilford Press. ISBN 978-1-60918-962-4. OCLC 713181786.
- ^ a b O'Connor, K., Aardema, F., & Pelissier, M.-C. (2005). Beyond reasonable doubt: Reasoning processes in obsessive-compulsive disorder and related disorders. Chichester: John Wiley & Sons.
- ^ Aardema, F., O'Connor, K. P., Emmelkamp, P. M., Marchand, A., & Todorov, C. (2005). Inferential confusion in obsessive-compulsive disorder: the inferential confusion questionnaire. Behaviour Research & Therapy, 43, 293-308.
- ^ O'Connor, K. (2002). Intrusions and inferences in obsessive compulsive disorder. Clinical Psychology & Psychotherapy, 9, 38-46.
- ^ O'Connor, K., & Aardema, F. (2012). Clinician's handbook for obsessive compulsive disorder: Inference-based therapy. Chichester: Wiley-Blackwell.
- ^ Aardema F, Bouchard S, Koszycki D, Lavoie ME, Audet JS, O'Connor K (2022). "Evaluation of Inference-Based Cognitive-Behavioral Therapy for Obsessive-Compulsive Disorder: A Multicenter Randomized Controlled Trial with Three Treatment Modalities". Psychotherapy and Psychosomatics. 91 (5): 348–359. doi:10.1159/000524425. ISSN 1423-0348. PMID 35584639. S2CID 248890026.
- ^ Koran LM, Hanna GL, Hollander E, Nestadt G, Simpson HB (July 2007). "Practice guideline for the treatment of patients with obsessive-compulsive disorder". The American Journal of Psychiatry. 164 (7 Suppl): 5–53. PMID 17849776.
- ^ Skapinakis P, Caldwell DM, Hollingworth W, Bryden P, Fineberg NA, Salkovskis P, et al. (August 2016). "Pharmacological and psychotherapeutic interventions for management of obsessive-compulsive disorder in adults: a systematic review and network meta-analysis". The Lancet. Psychiatry. 3 (8): 730–739. doi:10.1016/S2215-0366(16)30069-4. PMC 4967667. PMID 27318812.
- ^ Wheaton MG, DeSantis SM, Simpson HB (October 2016). "Network meta-analyses and treatment recommendations for obsessive-compulsive disorder". The Lancet. Psychiatry. 3 (10): 920. doi:10.1016/S2215-0366(16)30280-2. PMC 6690590. PMID 27692263.
- ^ Hirschtritt ME, Bloch MH, Mathews CA (April 2017). "Obsessive-Compulsive Disorder: Advances in Diagnosis and Treatment". JAMA. 317 (13): 1358–1367. doi:10.1001/jama.2017.2200. PMID 28384832. S2CID 13660201.
- ^ Simpson HB, Wetterneck CT, Cahill SP, Steinglass JE, Franklin ME, Leonard RC, et al. (1 March 2013). "Treatment of obsessive-compulsive disorder complicated by comorbid eating disorders". Cognitive Behaviour Therapy. 42 (1): 64–76. doi:10.1080/16506073.2012.751124. PMC 3947513. PMID 23316878.
- ^ "Antidepressants for children and teenagers: what works for anxiety and depression?". NIHR Evidence (Plain English summary). National Institute for Health and Care Research. 3 November 2022. doi:10.3310/nihrevidence_53342. S2CID 253347210.
- ^ Boaden K, Tomlinson A, Cortese S, Cipriani A (2 September 2020). "Antidepressants in Children and Adolescents: Meta-Review of Efficacy, Tolerability and Suicidality in Acute Treatment". Frontiers in Psychiatry. 11: 717. doi:10.3389/fpsyt.2020.00717. PMC 7493620. PMID 32982805.
- ^ Correll CU, Cortese S, Croatto G, Monaco F, Krinitski D, Arrondo G, et al. (June 2021). "Efficacy and acceptability of pharmacological, psychosocial, and brain stimulation interventions in children and adolescents with mental disorders: an umbrella review". World Psychiatry. 20 (2): 244–275. doi:10.1002/wps.20881. PMC 8129843. PMID 34002501.
- ^ Arroll B, Elley CR, Fishman T, Goodyear-Smith FA, Kenealy T, Blashki G, et al. (July 2009). Arroll B (ed.). "Antidepressants versus placebo for depression in primary care". The Cochrane Database of Systematic Reviews. 2009 (3): CD007954. doi:10.1002/14651858.CD007954. PMC 10576545. PMID 19588448.
- ^ "Review Finds SSRIs Modestly Effective in Short-Term Treatment of OCD". Archived from the original on 13 April 2013.
- ^ Fineberg NA, Brown A, Reghunandanan S, Pampaloni I (September 2012). "Evidence-based pharmacotherapy of obsessive-compulsive disorder". The International Journal of Neuropsychopharmacology. 15 (8): 1173–1191. doi:10.1017/S1461145711001829. hdl:2299/216. PMID 22226028.
- ^ "Sertraline prescribing information" (PDF). Archived (PDF) from the original on 16 June 2015. Retrieved 30 January 2015.
- ^ "Paroxetine prescribing information" (PDF). Archived from the original (PDF) on 19 February 2015. Retrieved 30 January 2015.
- ^ Pignon B, Tezenas du Montcel C, Carton L, Pelissolo A (November 2017). "The Place of Antipsychotics in the Therapy of Anxiety Disorders and Obsessive-Compulsive Disorders". Current Psychiatry Reports. 19 (12): 103. doi:10.1007/s11920-017-0847-x. PMID 29110139. S2CID 41312623.
- ^ Komossa K, Depping AM, Meyer M, Kissling W, Leucht S (December 2010). "Second-generation antipsychotics for obsessive compulsive disorder". The Cochrane Database of Systematic Reviews (12): CD008141. doi:10.1002/14651858.CD008141.pub2. PMID 21154394. S2CID 205193449.
- ^ Koran LM, Hanna GL, Hollander E, Nestadt G, Simpson HB (July 2007). "Practice guideline for the treatment of patients with obsessive-compulsive disorder" (PDF). The American Journal of Psychiatry. 164 (7 Suppl). American Psychiatric Association: 5–53. PMID 17849776.
- ^ Cybulska EM (February 2006). "Obsessive-compulsive disorder, the brain and electroconvulsive therapy". British Journal of Hospital Medicine. 67 (2): 77–81. doi:10.12968/hmed.2006.67.2.20466. PMID 16498907.
- ^ Perera MP, Mallawaarachchi S, Miljevic A, Bailey NW, Herring SE, Fitzgerald PB (October 2021). "Repetitive Transcranial Magnetic Stimulation for Obsessive-Compulsive Disorder: A Meta-analysis of Randomized, Sham-Controlled Trials". Biological Psychiatry. Cognitive Neuroscience and Neuroimaging. 6 (10): 947–960. doi:10.1016/j.bpsc.2021.03.010. PMID 33775927. S2CID 232408932.
- ^ Barlow, D. H. and V. M. Durand. Essentials of Abnormal Psychology. California: Thomson Wadsworth, 2006.
- ^ Bosanac P, Hamilton B, Lucak J, Castle D (2018). "Identity challenges and 'burden of normality' after DBS for severe OCD: a narrative case study". BMC Psychiatry. 18 (1): 186. doi:10.1186/s12888-018-1771-2. PMC 5998583. PMID 29895269.
- ^ Barlas S (8 April 2009). "FDA Approves Pioneering Treatment for Obsessive- Compulsive Disorder". Psychiatric Times. 26 (4). Archived from the original on 10 July 2009.
- ^ Surgical Procedures for Obsessive–Compulsive Disorder Archived 25 July 2008 at the Wayback Machine, by M. Jahn and M. Williams, PhD,. BrainPhysics OCD Resource, Accessed 6 July 2008.
- ^ O'Donohue W, Ferguson KE (2006). "Evidence-Based Practice in Psychology and Behavior Analysis". The Behavior Analyst Today. 7 (3): 335–347. doi:10.1037/h0100155.
- ^ a b Freeman J, Garcia A, Frank H, Benito K, Conelea C, Walther M, et al. (2014). "Evidence base update for psychosocial treatments for pediatric obsessive-compulsive disorder". Journal of Clinical Child and Adolescent Psychology. 43 (1): 7–26. doi:10.1080/15374416.2013.804386. PMC 3815743. PMID 23746138.
- ^ Rapoport JE (1989). Obsessive-compulsive Disorder in Children & Adolescents. Washington: American Psychiatric Press.
- ^ Adams PL (1973). Obsessive Children: A Sociopsychiatric Study. Philadelphia: Brunner / Mazel.
- ^ D'Alessandro TM (2009). "Factors influencing the onset of childhood obsessive compulsive disorder". Pediatric Nursing. 35 (1): 43–46. PMID 19378573.
- ^ Eddy KT, Dutra L, Bradley R, Westen D (December 2004). "A multidimensional meta-analysis of psychotherapy and pharmacotherapy for obsessive-compulsive disorder". Clinical Psychology Review. 24 (8): 1011–1030. doi:10.1016/j.cpr.2004.08.004. PMID 15533282. S2CID 6582600.
- ^ Subramaniam M, Soh P, Vaingankar JA, Picco L, Chong SA (May 2013). "Quality of life in obsessive-compulsive disorder: impact of the disorder and of treatment". CNS Drugs. 27 (5): 367–383. doi:10.1007/s40263-013-0056-z. PMID 23580175. S2CID 8038340.
- ^ Boileau B (2011). "A review of obsessive-compulsive disorder in children and adolescents". Dialogues in Clinical Neuroscience. 13 (4): 401–411. doi:10.31887/DCNS.2011.13.4/bboileau. PMC 3263388. PMID 22275846.
- ^ Thamby A, Khanna S (2019). "The role of personality disorders in obsessive-compulsive disorder". Indian Journal of Psychiatry. 61 (7): S114–S118. doi:10.4103/psychiatry.IndianJPsychiatry_526_18. PMC 6343421. PMID 30745684.
- ^ "Obsessive-Compulsive Disorder (OCD)". National Institute for Mental Health. September 2022. Retrieved 15 March 2023.
- ^ Summers J, Sinnott-Armstrong W (2019). "Obsessive Compulsive Disorder: A Little History". Clean Hands: Philosophical Lessons from Scrupulosity. Oxford University Press. p. 19. ISBN 978-0-19-005869-2.
- ^ Friedrich P (29 April 2016). The Literary and Linguistic Construction of Obsessive-Compulsive Disorder: No Ordinary Doubt. Springer. ISBN 978-1-137-42733-5.
- ^ Plutarch (1951). Selected Lives and Essays. Classics Club. p. 375.
- ^ a b c d e f g h i j k l m Osborn I (1998). Tormenting Thoughts and Secret Rituals: The Hidden Epidemic of Obsessive-Compulsive Disorder. New York City, New York: Dell Publishing. ISBN 978-0-440-50847-2.
- ^ a b Awaad R, Ali S (15 July 2015). "Obsessional Disorders in al-Balkhi's 9th century treatise: Sustenance of the Body and Soul". Journal of Affective Disorders. 180: 185–189. doi:10.1016/j.jad.2015.03.003. PMID 25911133.
- ^ Al-Balkhi A, Misri M, al-Hayyat M (2005). Masālih al-Abdān Wa-al-Anfus (in Arabic). Cairo: Ma'had al-Makhtūtāt al-'Arabīyah.
- ^ a b Jenike MA, Baer L, Minichiello WE (1986). Obsessive Compulsive Disorders: Theory and Management. Littleton, MA: PSG Publishing.
- ^ Berrios GE (1989). "Obsessive-compulsive disorder: its conceptual history in France during the 19th century". Comprehensive Psychiatry. 30 (4): 283–295. doi:10.1016/0010-440x(89)90052-7. PMID 2667880.
- ^ Freud S (1950). Totem and Taboo:Some Points of Agreement between the Mental Lives of Savages and Neurotics. Translated by Strachey J. New York: W. W. Norton & Company. p. 29. ISBN 978-0-393-00143-3.
- ^ Meyer V (1966). "Modification of expectations in cases with obsessional rituals". Behaviour Research and Therapy. 4 (4): 273–280. doi:10.1016/0005-7967(66)90023-4. PMID 5978682.
- ^ "Behavior Therapy for OCD: Its Origin".
- ^ Osborn I (1999). Tormenting Thoughts and Secret Rituals: The Hidden Epidemic of Obsessive-Compulsive Disorder. New York: Dell Publishing. ISBN 978-0-440-50847-2.
- ^ a b "The history of obsessive-compulsive disorder". ocdhistory.net. Retrieved 4 November 2023.
- ^ Guzick AG, Candelari A, Wiese AD, Schneider SC, Goodman WK, Storch EA (November 2021). "Obsessive–Compulsive Disorder During the COVID-19 Pandemic: a Systematic Review". Current Psychiatry Reports. 23 (11): 71. doi:10.1007/s11920-021-01284-2. PMC 8493778. PMID 34613498.
- ^ Penzel F. "Samuel Johnson (1709–1784): A Patron Saint of OCD?". International OCD Foundation. Archived from the original on 18 June 2005. Retrieved 29 November 2013 – via Westsuffolkpsych.homestead.com.
- ^ Waude A (29 March 2016). "Rat Man Case Study: Sigmund Freud's Search For The Cause Of One Man's Obsessive Thoughts". www.psychologistworld.com.
- ^ Dittmann M (July–August 2005). "Hughes's germ phobia revealed in psychological autopsy". American Psychological Association. Archived from the original on 5 January 2015. Retrieved 9 January 2015.
- ^ Dittmann M (July–August 2005). "Hughes's germ phobia revealed in psychological autopsy". Monitor on Psychology. 36 (7). Archived from the original on 29 December 2008.
- ^ Chosak A (12 October 2012). "The Aviator: A real-life portrayal of OCD in the media". Massachusetts General Hospital OCD and Related Disorders Program. Archived from the original on 22 February 2015. Retrieved 9 January 2015.
- ^ "George Ezra opens up about OCD struggle". BBC News. 31 August 2020.
- ^ "Greta Thunberg was nearly hospitalised due to disordered eating, says mother". Independent.co.uk. 24 February 2020.
- ^ Goldman A (21 April 2014). "James Spader: The Strangest Man on TV". Rolling Stone. Retrieved 10 July 2023.
- ^ "EXCLUSIVE: Chile's President On Why He's Open About His OCD". Amanpour and Company. 26 September 2022. Retrieved 10 July 2023 – via YouTube.
- ^ Banfield-Nwachi M (28 April 2023). "David Beckham reveals impact of OCD in new documentary". The Guardian.
- ^ Fennell D, Boyd M (2 September 2014). "Obsessive-Compulsive Disorder in the Media". Deviant Behavior. 35 (9): 669–686. doi:10.1080/01639625.2013.872526. ISSN 0163-9625. S2CID 145735144.
- ^ "Don't Be Afraid of the Word "Disorder"". Beyond OCD. Retrieved 11 November 2020.
- ^ Goldberg FR (2007). Turn box office movies into mental health opportunities: A literature review and resource guide for clinicians and educators (PDF). Beneficial Film Guides, Inc. p. 8. Archived from the original (PDF) on 8 July 2011. Retrieved 17 February 2010.
- ^ "Felix Unger from The Odd Couple". CharacTour.
- ^ Berman N (5 October 2012). "Is This 'As Good as It Gets?': Popular Media's Representation of OCD". Massachusetts General Hospital OCD and Related Disorders Program. Archived from the original on 22 February 2015. Retrieved 9 January 2015.
- ^ Almeida J. "Royal College of Psychiatrists, Discover Psychiatry, Minds on Film Blog, Matchstick Men". Royal College of Psychiatrists. Archived from the original on 22 February 2015. Retrieved 14 January 2015.
- ^ Stewart S (16 September 2007). "Happy to Be Neurotic, at Least Once a Week". The New York Times. Archived from the original on 11 December 2008. Retrieved 8 December 2008.
- ^ Anxiety Disorders Association of America. "What Is OCD?". USA Network. Archived from the original on 17 December 2008. Retrieved 8 December 2008.
- ^ Gioia M (6 April 2016). "Double Dare Host Marc Summers Crossed Paths With Broadway, and Now He's Got a Solo Show". Playbill. Retrieved 27 February 2024.
- ^ Flood A (14 October 2017). "John Green: 'Having OCD is an ongoing part of my life'". The Guardian. Retrieved 21 September 2019.
- ^ Mangan L (30 January 2019). "Pure review – a masterly comedy about sex and mental health". The Guardian. Retrieved 7 April 2021.
- ^ Camfield DA, Sarris J, Berk M (June 2011). "Nutraceuticals in the treatment of obsessive compulsive disorder (OCD): a review of mechanistic and clinical evidence". Progress in Neuro-Psychopharmacology & Biological Psychiatry. 35 (4): 887–895. doi:10.1016/j.pnpbp.2011.02.011. PMID 21352883. S2CID 30024004.
- ^ Davidson J, Bjorgvinsson T (June 2003). "Current and potential pharmacological treatments for obsessive-compulsive disorder". Expert Opinion on Investigational Drugs. 12 (6): 993–1001. doi:10.1517/13543784.12.6.993. PMID 12783603. S2CID 35971588.
- ^ Koran LM (2007). "Obsessive-Compulsive Disorder: An Update for the Clinician". Focus (5): 3.
- ^ Wu K, Hanna GL, Rosenberg DR, Arnold PD (February 2012). "The role of glutamate signaling in the pathogenesis and treatment of obsessive-compulsive disorder". Pharmacology, Biochemistry, and Behavior. 100 (4): 726–735. doi:10.1016/j.pbb.2011.10.007. PMC 3437220. PMID 22024159.
- ^ Ranjan S, Gautam A (2023). "Pharmaceutical prospects of Silymarin for the treatment of neurological patients: an updated insight". Frontiers in Neuroscience. 17. doi:10.3389/fnins.2023.1159806. ISSN 1662-453X. PMC 10232807. PMID 37274201.
External links
- National Institute Of Mental Health
- American Psychiatric Association
- APA Division 12 treatment page for obsessive-compulsive disorder
- Davis LJ (2008). Obsession: A History. University of Chicago Press. ISBN 978-0-226-13782-7.
